Patient Protection and Affordable Care Act

 Clash Royale CLAN TAG#URR8PPP
Clash Royale CLAN TAG#URR8PPP  | |
| Long title | The Patient Protection and Affordable Care Act |
|---|---|
Acronyms (colloquial) | PPACA, ACA |
| Nicknames | Obamacare, Affordable Care Act, Health Insurance Reform, Healthcare Reform |
| Enacted by | the 111th United States Congress |
| Effective | March 23, 2010 (2010-03-23) Most major provisions phased in by January 2014; remaining provisions phased in by 2020; individual mandate repealed starting 2019 |
| Citations | |
| Public law | 111–148 |
| Statutes at Large | 124 Stat. 119 through 124 Stat. 1025 (906 pages) |
| Legislative history | |
| |
| Major amendments | |
Health Care and Education Reconciliation Act of 2010 Comprehensive 1099 Taxpayer Protection and Repayment of Exchange Subsidy Overpayments Act of 2011 Public Law 115-97 proposed as the Tax Cuts and Jobs Act of 2017 | |
United States Supreme Court cases | |
National Federation of Independent Business v. Sebelius Burwell v. Hobby Lobby King v. Burwell | |
| ||
|---|---|---|
Pre-presidency
44th President of the United States
Policies
Appointments
First term
Second term
Post-presidency
 | ||
The Patient Protection and Affordable Care Act, often shortened to the Affordable Care Act (ACA) or nicknamed Obamacare, is a United States federal statute enacted by the 111th United States Congress and signed into law by President Barack Obama on March 23, 2010. The term "Obamacare" was first used by opponents, then reappropriated by supporters, and eventually used by President Obama himself.[1] Together with the Health Care and Education Reconciliation Act of 2010 amendment, it represents the U.S. healthcare system's most significant regulatory overhaul and expansion of coverage since the passage of Medicare and Medicaid in 1965.[2][3][4][5]
The ACA's major provisions came into force in 2014. By 2016, the uninsured share of the population had roughly halved, with estimates ranging from 20 to 24 million additional people covered during 2016.[6][7] The increased coverage was due, roughly equally, to an expansion of Medicaid eligibility and to major changes to individual insurance markets. Both involved new spending, funded through a combination of new taxes and cuts to Medicare provider rates and Medicare Advantage. Several Congressional Budget Office reports said that overall these provisions reduced the budget deficit, that repealing the ACA would increase the deficit,[8][9] and that the law reduced income inequality by taxing primarily the top 1% to fund roughly $600 in benefits on average to families in the bottom 40% of the income distribution.[10] The law also enacted a host of delivery system reforms intended to constrain healthcare costs and improve quality. After the law went into effect, increases in overall healthcare spending slowed, including premiums for employer-based insurance plans.[11]
The act largely retains the existing structure of Medicare, Medicaid, and the employer market, but individual markets were radically overhauled around a three-legged scheme.[2][12] Insurers in these markets are made to accept all applicants and charge the same rates regardless of pre-existing conditions or sex. To combat resultant adverse selection, the act mandates that individuals buy insurance and insurers cover a list of "essential health benefits". However, a repeal of the tax mandate, passed as part of the Tax Cuts and Jobs Act of 2017, will become effective in 2019. To help households between 100–400% of the Federal Poverty Line afford these compulsory policies, the law provides insurance premium subsidies. Other individual market changes include health marketplaces and risk adjustment programs.
The act has also faced challenges and opposition. The Supreme Court ruled 5 to 4 in 2012 that states could choose not to participate in the ACA's Medicaid expansion, although it upheld the law as a whole.[13] The federal health exchange, HealthCare.gov, faced major technical problems at the beginning of its rollout in 2013. In 2017, a unified Republican government failed to pass several different partial repeals of the ACA. The law spent several years opposed by a slim plurality of Americans polled, although its provisions were generally more popular than the law as a whole,[14] and the law gained majority support by 2017.[15]
Contents
1 Provisions
1.1 Insurance regulations
1.2 Individual mandate
1.3 Subsidies
1.4 Exchanges
1.5 Risk corridor program
1.6 Temporary reinsurance
1.7 Risk adjustment
1.8 Medicaid expansion
1.9 Medicare savings
1.10 Taxes
1.10.1 Medicare taxes
1.10.2 Excise taxes
1.11 SCHIP
1.12 Dependent's Health Insurance
1.13 Employer mandate
1.14 Delivery system reforms
1.14.1 Hospital quality
1.14.2 Bundled Payments
1.14.3 Accountable Care Organizations
1.15 Medicare donut hole
1.16 State waivers
1.17 Other insurance provisions
1.18 Menu calorie listings
2 Legislative history
2.1 Background
2.2 Healthcare debate, 2008–10
2.2.1 Senate
2.2.2 House
3 Impact
3.1 Coverage
3.2 Taxes
3.3 Insurance exchanges
3.4 Medicaid expansion
3.5 Healthcare insurance costs
3.5.1 Effect on deductibles and co-payments
3.6 Health outcomes
3.7 Distributional impact
3.8 Federal deficit
3.8.1 CBO estimates of revenue and impact on deficit
3.8.2 Opinions on CBO projections
3.9 Economic consequences
3.10 Employer mandate and part-time work
3.11 Hospitals
4 Public opinion
5 Political aspects
5.1 "Obamacare"
5.2 Common misconceptions
5.2.1 "Death panels"
5.2.2 Members of Congress
5.2.3 Illegal immigrants
5.2.4 Exchange "death spiral"
6 Opposition
6.1 Legal challenges
6.1.1 National Federation of Independent Business v. Sebelius
6.1.2 Contraception mandate
6.1.3 House v. Price
6.1.4 Non-cooperation
6.2 Repeal efforts
6.2.1 2013 federal government shutdown
6.2.2 2017 repeal effort
6.3 Actions to hinder implementation
6.4 Ending cost-sharing reduction (CSR) payments
7 Implementation
7.1 Murray—Alexander Individual Market Stabilization Bill
8 See also
9 References
10 Further reading
10.1 Preliminary CBO documents
10.2 CMS Estimates of the impact of P.L. 111-148
10.3 CMS Estimates of the impact of H.R. 3590
10.4 Senate Finance Committee meetings
11 External links
11.1 PPACA text
Provisions

The President and White House Staff react to the House of Representatives passing the bill on March 21, 2010.

Jim Clyburn and Nancy Pelosi celebrating after the House passes the amended bill on March 21
The ACA includes provisions to take effect from 2010 to 2020, although most took effect on January 1, 2014. It amended the Public Health Service Act of 1944 and inserted new provisions on affordable care into Title 42 of the United States Code.[citation needed] Few areas of the US health care system were left untouched, making it the most sweeping health care reform since the enactment of Medicare and Medicaid in 1965.[2][3][4][16][5] However, some areas were more affected than others. The individual insurance market was radically overhauled, and many of the law's regulations applied specifically to this market,[2] while the structure of Medicare, Medicaid, and the employer market were largely retained.[3] Most of the coverage gains were made through the expansion of Medicaid,[17] and the biggest cost savings were made in Medicare.[3] Some regulations applied to the employer market, and the law also made delivery system changes that affected most of the health care system.[3] Not all provisions took full effect. Some were made discretionary, some were deferred, and others were repealed before implementation.
Insurance regulations
Guaranteed issue prohibits insurers from denying coverage to individuals due to pre-existing conditions. States were required to ensure the availability of insurance for individual children who did not have coverage via their families.- Premiums must be the same for everyone of a given age, regardless of preexisting conditions. Premiums are allowed to vary by enrollee age, but those for the oldest enrollees (age 45–64, average expenses $5,542) can only be three times as large as those for adults 18–24 ($1,836).[18]
Essential health benefits must be provided. The National Academy of Medicine defines the law's "essential health benefits" as "ambulatory patient services; emergency services; hospitalization; maternity and newborn care; mental health and substance use disorder services, including behavioral health treatment; prescription drugs; rehabilitative and habilitative services and devices; laboratory services; preventive and wellness services and chronic disease management; and pediatric services, including oral and vision care"[19][20][21][22][23][24][25] and others[26] rated Level A or B by the U.S. Preventive Services Task Force.[27] In determining what would qualify as an essential benefit, the law required that standard benefits should offer at least that of a "typical employer plan".[24] States may require additional services.[28]- Additional preventive care and screenings for women.[29] The guidelines issued by the Health Resources and Services Administration to implement this provision mandate "[a]ll Food and Drug Administration approved contraceptive methods, sterilization procedures, and patient education and counseling for all women with reproductive capacity".[30] This mandate applies to all employers and educational institutions except for religious organizations.[31][32] These regulations were included on the recommendations of the Institute of Medicine.[33][34]

In 2012 Senator Sheldon Whitehouse created this summary to explain his view on the act.
- Annual and lifetime coverage caps on essential benefits were banned.[35][36]
- Prohibits insurers from dropping policyholders when they get sick.[37]
- All health policies sold in the United States must provide an annual maximum out of pocket (MOOP) payment cap for an individual's or family's medical expenses (excluding premiums). After the MOOP payment cap is reached, all remaining costs must be paid by the insurer.[38]
- A partial community rating requires insurers to offer the same premium to all applicants of the same age and location without regard to gender or most pre-existing conditions (excluding tobacco use).[39][40][41] Premiums for older applicants can be no more than three times those for the youngest.[42]
- Preventive care, vaccinations and medical screenings cannot be subject to co-payments, co-insurance or deductibles.[43][44][45] Specific examples of covered services include: mammograms and colonoscopies, wellness visits, gestational diabetes screening, HPV testing, STI counseling, HIV screening and counseling, contraceptive methods, breastfeeding support/supplies and domestic violence screening and counseling.[46]
- The law established four tiers of coverage: bronze, silver, gold and platinum. All categories offer the essential health benefits. The categories vary in their division of premiums and out-of-pocket costs: bronze plans have the lowest monthly premiums and highest out-of-pocket costs, while platinum plans are the reverse.[24][47] The percentages of health care costs that plans are expected to cover through premiums (as opposed to out-of-pocket costs) are, on average: 60% (bronze), 70% (silver), 80% (gold), and 90% (platinum).[48]
- Insurers are required to implement an appeals process for coverage determination and claims on all new plans.[37]
- Insurers must spend at least 80–85% of premium dollars on health costs; rebates must be issued to policyholders if this is violated.[49][50]
Individual mandate
The individual mandate[51] was the requirement to buy insurance or pay a penalty for everyone not covered by an employer sponsored health plan, Medicaid, Medicare or other public insurance programs (such as Tricare). Also exempt were those facing a financial hardship or who were members in a recognized religious sect exempted by the Internal Revenue Service.[52]
The mandate and the limits on open enrollment[53][54] were designed to avoid the insurance death spiral in which healthy people delay insuring themselves until they get sick. In such a situation, insurers would have to raise their premiums to cover the relatively sicker and thus more expensive policies,[51][55][56] which could create a vicious cycle in which more and more people drop their coverage.[57]
The purpose of the mandate was to prevent the healthcare system from succumbing to adverse selection, which would result in high premiums for the insured and little coverage (and thus more illness and medical bankruptcy) for the uninsured.[55][58][59] Studies by the CBO, Gruber and Rand Health concluded that a mandate was required.[60][61][62] The mandate increased the size and diversity of the insured population, including more young and healthy participants to broaden the risk pool, spreading costs.[63] Experience in New Jersey and Massachusetts offered divergent outcomes.[58][61][64]
Among the groups who were not subject to the individual mandate are:
Illegal immigrants, estimated at around 8 million—or roughly a third of the 23 million projection—are ineligible for insurance subsidies and Medicaid.[65][66] They remain eligible for emergency services.- Eligible citizens not enrolled in Medicaid.[67]
- Citizens who pay the annual penalty instead of purchasing insurance, mostly younger and single.[67]
- Citizens whose insurance coverage would cost more than 8% of household income and are exempt from the penalty.[67]
- Citizens who live in states that opt out of the Medicaid expansion and who qualify for neither existing Medicaid coverage nor subsidized coverage through the states' new insurance exchanges.[68]
- All citizens as of December 20, 2017[69]
On December 20, 2017, the individual mandate was repealed starting in 2019 via the Tax Cuts and Jobs Act of 2017.[69]
Subsidies
Households with incomes between 100% and 400% of the federal poverty level are eligible to receive federal subsidies for policies purchased via an exchange.[70][71] Subsidies are provided as an advanceable, refundable tax credits.[72][73] Additionally, small businesses are eligible for a tax credit provided that they enroll in the SHOP Marketplace.[74] Under the law, workers whose employers offer affordable coverage will not be eligible for subsidies via the exchanges. To be eligible the cost of employer-based health insurance must exceed 9.5% of the worker's household income.
| Income % of federal poverty level | Premium Cap as a Share of Income | Incomea | Max Annual Out-of-Pocket Premium | Premium Savingsb | Additional Cost-Sharing Subsidy |
|---|---|---|---|---|---|
| 133% | 3% of income | $31,900 | $992 | $10,345 | $5,040 |
| 150% | 4% of income | $33,075 | $1,323 | $9,918 | $5,040 |
| 200% | 6.3% of income | $44,100 | $2,778 | $8,366 | $4,000 |
| 250% | 8.05% of income | $55,125 | $4,438 | $6,597 | $1,930 |
| 300% | 9.5% of income | $66,150 | $6,284 | $4,628 | $1,480 |
| 350% | 9.5% of income | $77,175 | $7,332 | $3,512 | $1,480 |
| 400% | 9.5% of income | $88,200 | $8,379 | $2,395 | $1,480 |
a.^ Note: In 2014, the FPL was $11,800 for a single person and $24,000 for family of four.[80][81] See Subsidy Calculator for specific dollar amount.[82] | |||||
Exchanges
Established the creation of health insurance exchanges in all fifty states. The exchanges are regulated, largely online marketplaces, administered by either federal or state government, where individuals and small business can purchase private insurance plans.[83][84][85]
Setting up an exchange gives a state partial discretion on standards and prices of insurance.[86][87] For example, states approve plans for sale, and influence (through limits on and negotiations with private insurers) the prices on offer. They can impose higher or state-specific coverage requirements—including whether plans offered in the state can cover abortion.[88] States without an exchange do not have that discretion. The responsibility for operating their exchanges moves to the federal government.[86]
Risk corridor program
This section contains too many or too-lengthy quotations for an encyclopedic entry. (July 2017) |
The risk-corridor program was a temporary risk management device defined under the PPACA section 1342[89]:1
to encourage reluctant insurers into the "new and untested"[attribution needed] ACA insurance market during the first three years that ACA was implemented (2014–2016). For those years the Department of Health and Human Services (HHS) "would cover some of the losses for insurers whose plans performed worse than they expected. Insurers that were especially profitable, for their part, would have to return to HHS some of the money they earned on the exchanges"[90][91][attribution needed]
According to an article in Forbes, risk corridors "had been a successful part of the Medicare prescription drug benefit, and the ACA's risk corridors were modeled after Medicare's Plan D."[92] They operated on the principle that "more participation would mean more competition, which would drive down premiums and make health insurance more affordable"[attribution needed] and "[w]hen insurers signed up to sell health plans on the exchanges, they did so with the expectation that the risk-corridor program would limit their downside losses."[90][attribution needed] The risk corridors succeeded in attracting ACA insurers. The program did not pay for itself as planned with "accumulated losses"[attribution needed] up to $8.3 billion for 2014 and 2015 alone. Authorization had to be given so that HHS could pay insurers from "general government revenues".[attribution needed] Congressional Republicans "railed against"[attribution needed] the program as a 'bailout' for insurers. Then-Rep. Jack Kingston (R-Ga.), on the Appropriations Committee that funds the Department of Health and Human Services and the Labor Department "[slipped] in a sentence"—Section 227—in the "massive" appropriations Consolidated Appropriations Act, 2014 (H.R. 3547) that said that no funds in the discretionary spending bill "could be used for risk-corridor payments."[attribution needed] This effectively "blocked the administration from obtaining the necessary funds from other programs"[93][attribution needed] and placed Congress in a potential breach of contract with insurers who offered qualified health plans, under the Tucker Act[89] as it did not pay the insurers.[94][94]
On February 10, 2017, in the Moda Health v the US Government, Moda, one of the insurers that struggled financially because of the elimination of the risk corridor program, won a "$214-million judgment against the federal government".[attribution needed] On appeal, judge Thomas C. Wheeler stated, "the Government made a promise in the risk corridors program that it has yet to fulfill. Today, the court directs the Government to fulfill that promise. After all, to say to [Moda], 'The joke is on you. You shouldn't have trusted us,' is hardly worthy of our great government."[95]
Temporary reinsurance
Temporary reinsurance for insurance for insurers against unexpectedly high claims was a program that ran from 2014 through 2016. It was intended to limit insurer losses.[citation needed]
Risk adjustment
Of the three risk management programs, only risk adjustment was permanent. Risk adjustment attempts to spread risk among insurers to prevent purchasers with good knowledge of their medical needs from using insurance to cover their costs (adverse selection). Plans with low actuarial risk compensate plans with high actuarial risk.[citation needed]
Medicaid expansion
ACA revised and expanded Medicaid eligibility starting in 2014. Under the law as written, all U.S. citizens and legal residents with income up to 133% of the poverty line, including adults without dependent children, would qualify for coverage in any state that participated in the Medicaid program. The federal government paid 100% of the cost of Medicaid eligibility expansion in participating states in 2014, 2015, and 2016; and will pay 95% in 2017, 94% in 2018, 93% in 2019, and 90% in 2020 and all subsequent years.[96][97][98] The law provides a 5% "income disregard", making the effective income eligibility limit for Medicaid 138% of the poverty level.[99]
However, the Supreme Court ruled in NFIB v. Sebelius that this provision of the ACA was coercive, and that the federal government must allow states to continue at pre-ACA levels of funding and eligibility if they chose.
Medicare savings
Spending reductions included a reduction in Medicare reimbursements to insurers and drug companies for private Medicare Advantage policies that the Government Accountability Office and Medicare Payment Advisory Commission found to be excessively costly relative to government Medicare;[100][101] and reductions in Medicare reimbursements to hospitals that failed standards of efficiency and care.[100]
Taxes
Medicare taxes
Income from self-employment and wages of single individuals in excess of $200,000 annually are subject to an additional tax of 0.9%. The threshold amount is $250,000 for a married couple filing jointly (threshold applies to joint compensation of the two spouses), or $125,000 for a married person filing separately.[102]
In the ACA's companion legislation, the Health Care and Education Reconciliation Act of 2010, an additional Medicare tax of 3.8% was applied to unearned income, specifically the lesser of net investment income or the amount by which adjusted gross income exceeds $200,000 ($250,000 for a married couple filing jointly; $125,000 for a married person filing separately.)[103]
Excise taxes
Excise taxes for the Affordable Care Act raised $16.3 billion in fiscal year 2015 (17% of all excise taxes collected by the Federal Government). $11.3 billion was raised by an excise tax placed directly on health insurers based on their market share. The ACA also includes an excise tax of 40% ("Cadillac tax") on total employer premium spending in excess of specified dollar amounts ($10,200 for single coverage and $27,500 for family coverage[104]) indexed to inflation, originally scheduled to take effect in 2018, but delayed until 2020 by the Consolidated Appropriations Act, 2016. Annual excise taxes totaling $3 billion were levied on importers and manufacturers of prescription drugs. An excise tax of 2.3% on medical devices and a 10% excise tax on indoor tanning services were applied as well.[105]
SCHIP
The State Children's Health Insurance Program (CHIP) enrollment process was simplified.[106]
Dependent's Health Insurance
Dependents were permitted to remain on their parents' insurance plan until their 26th birthday, including dependents who no longer live with their parents, are not a dependent on a parent's tax return, are no longer a student, or are married.[107][108]
Employer mandate
Businesses that employ 50 or more people but do not offer health insurance to their full-time employees pay a tax penalty if the government has subsidized a full-time employee's healthcare through tax deductions or other means. This is commonly known as the employer mandate.[109][110] This provision was included to encourage employers to continue providing insurance once the exchanges began operating.[111] Approximately 44% of the population was covered directly or indirectly through an employer.[112][113]
Delivery system reforms
The act includes a host of delivery system reforms intended to constrain healthcare costs and improve quality. These include Medicare payment changes to discourage hospital-acquired conditions and readmissions, bundled payment initiatives, the Center for Medicare and Medicaid Innovation, the Independent Payment Advisory Board, and the creation of Accountable care organizations.
Hospital quality
Health care cost/quality initiatives including incentives to reduce hospital infections, to adopt electronic medical records, and to coordinate care and prioritize quality over quantity.[114]
The Hospital Readmissions Reduction Program (HRPP) was established as an addition to the Social Security Act, in an effort to reduce hospital readmissions. This program penalizes hospitals with higher than expected readmission rates by decreasing their Medicare reimbursement rate.
Bundled Payments
The Medicare payment system switched from fee-for-service to bundled payments.[115][116] A single payment was to be paid to a hospital and a physician group for a defined episode of care (such as a hip replacement) rather than individual payments to individual service providers. In addition, the Medicare Part D coverage gap (commonly called the "donut hole") was to shrink incrementally, closing completely by January 1, 2020.[117]
Accountable Care Organizations
The Act allowed the creation of Accountable Care Organizations (ACOs), which are groups of doctors, hospitals and other providers that commit to give coordinated, high quality care to Medicare patients. ACOs were allowed to continue using a fee for service billing approach. They receive bonus payments from the government for minimizing costs while achieving quality benchmarks that emphasize prevention and mitigation of chronic disease. If they fail to do so, they are subject to penalties.[118]
Unlike Health Maintenance Organizations, ACO patients are not required to obtain all care from the ACO. Also, unlike HMOs, ACOs must achieve quality of care goals.[118]
Medicare donut hole
Medicare Part D participants received a 50% discount on brand name drugs purchased after exhausting their initial coverage and before reaching the catastrophic-coverage threshold.[119] The United States Department of Health and Human Services began mailing rebate checks in 2010.[120] By the year 2020, the donut hole will be completely phased out.[121]
State waivers
From 2017 onwards, states can apply for a "waiver for state innovation" that allows them to conduct experiments that meet certain criteria.[122] To obtain a waiver, a state must pass legislation setting up an alternative health system that provides insurance at least as comprehensive and as affordable as ACA, covers at least as many residents and does not increase the federal deficit.[123] These states can be exempt from some of ACA's central requirements, including the individual and employer mandates and the provision of an insurance exchange.[124] The state would receive compensation equal to the aggregate amount of any federal subsidies and tax credits for which its residents and employers would have been eligible under ACA plan, if they cannot be paid under the state plan.[122]
In May 2011, Vermont enacted Green Mountain Care, a state-based single-payer system for which they intended to pursue a waiver to implement.[125][126][127] In December 2014, Vermont decided not to continue due to high expected costs.[128]
Other insurance provisions
- The Community Living Assistance Services and Supports Act (or CLASS Act) established a voluntary and public long-term care insurance option for employees,[129][130][131]
- Consumer Operated and Oriented Plans (CO-OP), member-governed non-profit insurers, could start providing health care coverage, based on a 5-year federal loan.[132]
Menu calorie listings
Nutrition labeling requirements of the Affordable Care Act were signed into federal law in 2010, but implementation was delayed by the FDA several times until they went into effect on May 7, 2018.[133]
Legislative history

President Obama signing the Patient Protection and Affordable Care Act on March 23, 2010
Background
An individual mandate coupled with subsidies for private insurance as a means for universal healthcare was considered the best way to win the support of the Senate because it had been included in prior bipartisan reform proposals. The concept goes back to at least 1989, when the conservative The Heritage Foundation proposed an individual mandate as an alternative to single-payer health care.[134][135] It was championed for a time by conservative economists and Republican senators as a market-based approach to healthcare reform on the basis of individual responsibility and avoidance of free rider problems. Specifically, because the 1986 Emergency Medical Treatment and Active Labor Act (EMTALA) requires any hospital participating in Medicare (nearly all do) to provide emergency care to anyone who needs it, the government often indirectly bore the cost of those without the ability to pay.[136][137][138]
President Bill Clinton proposed a healthcare reform bill in 1993 that included a mandate for employers to provide health insurance to all employees through a regulated marketplace of health maintenance organizations. Republican Senators proposed an alternative that would have required individuals, but not employers, to buy insurance.[137] Ultimately the Clinton plan failed amid an unprecedented barrage of negative advertising funded by politically conservative groups and the health insurance industry and due to concerns that it was overly complex.[139] Clinton negotiated a compromise with the 105th Congress to instead enact the State Children's Health Insurance Program (SCHIP) in 1997.[140]

John Chafee
The 1993 Republican alternative, introduced by Senator John Chafee as the Health Equity and Access Reform Today Act, contained a "universal coverage" requirement with a penalty for noncompliance—an individual mandate—as well as subsidies to be used in state-based 'purchasing groups'.[141] Advocates for the 1993 bill included prominent Republicans such as Senators Orrin Hatch, Chuck Grassley, Bob Bennett and Kit Bond.[142][143] Of 1993's 43 Republican Senators, 20 supported the HEART Act.[134][144] Another Republican proposal, introduced in 1994 by Senator Don Nickles (R-OK), the Consumer Choice Health Security Act, contained an individual mandate with a penalty provision;[145] however, Nickles subsequently removed the mandate from the bill, stating he had decided "that government should not compel people to buy health insurance".[146] At the time of these proposals, Republicans did not raise constitutional issues with the mandate; Mark Pauly, who helped develop a proposal that included an individual mandate for George H. W. Bush, remarked, "I don't remember that being raised at all. The way it was viewed by the Congressional Budget Office in 1994 was, effectively, as a tax."[134]

Mitt Romney's Massachusetts went from 90% of its residents insured to 98%, the highest rate in the nation.[147]
In 2006, an insurance expansion bill was enacted at the state level in Massachusetts. The bill contained both an individual mandate and an insurance exchange. Republican Governor Mitt Romney vetoed the mandate, but after Democrats overrode his veto, he signed it into law.[148] Romney's implementation of the 'Health Connector' exchange and individual mandate in Massachusetts was at first lauded by Republicans. During Romney's 2008 presidential campaign, Senator Jim DeMint praised Romney's ability to "take some good conservative ideas, like private health insurance, and apply them to the need to have everyone insured". Romney said of the individual mandate: "I'm proud of what we've done. If Massachusetts succeeds in implementing it, then that will be the model for the nation."[149]
In 2007, a year after the Massachusetts reform, Republican Senator Bob Bennett and Democratic Senator Ron Wyden introduced the Healthy Americans Act, which featured an individual mandate and state-based, regulated insurance markets called "State Health Help Agencies".[138][149] The bill initially attracted bipartisan support, but died in committee. Many of the sponsors and co-sponsors remained in Congress during the 2008 healthcare debate.[150]
By 2008 many Democrats were considering this approach as the basis for healthcare reform. Experts said that the legislation that eventually emerged from Congress in 2009 and 2010 bore similarities to the 2007 bill[141] and that it was deliberately patterned after Romney's state healthcare plan.[151]
Healthcare debate, 2008–10
Healthcare reform was a major topic during the 2008 Democratic presidential primaries. As the race narrowed, attention focused on the plans presented by the two leading candidates, Hillary Clinton and the eventual nominee, Barack Obama. Each candidate proposed a plan to cover the approximately 45 million Americans estimated to not have health insurance at some point each year. Clinton's proposal would have required all Americans to obtain coverage (in effect, an individual mandate), while Obama's proposal provided a subsidy but rejected the use of an individual mandate.[152][153]
During the general election, Obama said that fixing healthcare would be one of his top four priorities as president.[154] Obama and his opponent, Sen. John McCain, proposed health insurance reforms though they differed greatly. Senator John McCain proposed tax credits for health insurance purchased in the individual market, which was estimated to reduce the number of uninsured people by about 2 million by 2018. Obama proposed private and public group insurance, income-based subsidies, consumer protections, and expansions of Medicaid and SCHIP, which was estimated at the time to reduce the number of uninsured people by 33.9 million by 2018.[155]

President Obama addressing Congress regarding healthcare reform, September 9, 2009
After his inauguration, Obama announced to a joint session of Congress in February 2009 his intent to work with Congress to construct a plan for healthcare reform.[156][157] By July, a series of bills were approved by committees within the House of Representatives.[158] On the Senate side, from June to September, the Senate Finance Committee held a series of 31 meetings to develop a healthcare reform bill. This group—in particular, Democrats Max Baucus, Jeff Bingaman and Kent Conrad, along with Republicans Mike Enzi, Chuck Grassley and Olympia Snowe—met for more than 60 hours, and the principles that they discussed, in conjunction with the other committees, became the foundation of the Senate healthcare reform bill.[159][160][161]
Congressional Democrats and health policy experts like MIT economics professor Jonathan Gruber[162] and David Cutler argued that guaranteed issue would require both community rating and an individual mandate to ensure that adverse selection and/or "free riding" would not result in an insurance "death spiral".[163] This approach was taken because the president and congressional leaders had concluded that more progressive plans, such as the (single-payer) Medicare for All act, could not obtain filibuster-proof support in the Senate. By deliberately drawing on bipartisan ideas—the same basic outline was supported by former Senate majority leaders Howard Baker, Bob Dole, Tom Daschle and George J. Mitchell—the bill's drafters hoped to garner the votes necessary for passage.[164][165]
However, following the adoption of an individual mandate, Republicans came to oppose the mandate and threatened to filibuster any bills that contained it.[134] Senate minority leader Mitch McConnell, who led the Republican congressional strategy in responding to the bill, calculated that Republicans should not support the bill, and worked to prevent defections:[166]
.mw-parser-output .templatequoteoverflow:hidden;margin:1em 0;padding:0 40px.mw-parser-output .templatequote .templatequoteciteline-height:1.5em;text-align:left;padding-left:1.6em;margin-top:0
It was absolutely critical that everybody be together because if the proponents of the bill were able to say it was bipartisan, it tended to convey to the public that this is O.K., they must have figured it out.[167]
Republican Senators, including those who had supported previous bills with a similar mandate, began to describe the mandate as "unconstitutional". Journalist Ezra Klein wrote in The New Yorker that "a policy that once enjoyed broad support within the Republican Party suddenly faced unified opposition."[138] Reporter Michael Cooper of The New York Times wrote that: "the provision ... requiring all Americans to buy health insurance has its roots in conservative thinking."[137][144]

Tea Party protesters at the Taxpayer March on Washington, September 12, 2009
The reform negotiations also attracted attention from lobbyists,[168] including deals between certain lobby groups and the advocates of the law to win the support of groups that had opposed past reforms, as in 1993.[169][170] The Sunlight Foundation documented many of the reported ties between "the healthcare lobbyist complex" and politicians in both parties.[171]
During the August 2009 summer congressional recess, many members went back to their districts and held town hall meetings on the proposals. The nascent Tea Party movement organized protests and many conservative groups and individuals attended the meetings to oppose the proposed reforms.[157] Many threats were made against members of Congress over the course of the debate.[172][173]
When Congress returned from recess, in September 2009 President Obama delivered a speech to a joint session of Congress supporting the ongoing Congressional negotiations.[174] He acknowledged the polarization of the debate, and quoted a letter from the late Senator Edward "Ted" Kennedy urging on reform: "what we face is above all a moral issue; that at stake are not just the details of policy, but fundamental principles of social justice and the character of our country."[175] On November 7, the House of Representatives passed the Affordable Health Care for America Act on a 220–215 vote and forwarded it to the Senate for passage.[157]
Senate
The Senate began work on its own proposals while the House was still working. The United States Constitution requires all revenue-related bills to originate in the House.[176] To formally comply with this requirement, the Senate used H.R. 3590, a bill regarding housing tax changes for service members.[177] It had been passed by the House as a revenue-related modification to the Internal Revenue Code. The bill became the Senate's vehicle for its healthcare reform proposal, discarding the bill's original content.[178] The bill ultimately incorporated elements of proposals that were reported favorably by the Senate Health and Finance committees. With the Republican Senate minority vowing to filibuster, 60 votes would be necessary to pass the Senate.[179] At the start of the 111th Congress, Democrats had only 58 votes; the Senate seat in Minnesota ultimately won by Al Franken was still undergoing a recount, while Arlen Specter was still a Republican (he became a Democrat in April, 2009).
Negotiations were undertaken attempting to satisfy moderate Democrats and to bring Republican senators aboard; particular attention was given to Republicans Bennett, Enzi, Grassley and Snowe. On July 7 Franken was sworn into office, providing a potential 60th vote. On August 25 Ted Kennedy—a longtime healthcare reform advocate—died. Paul Kirk was appointed as Senator Kennedy's temporary replacement on September 24.
After the Finance Committee vote on October 15, negotiations turned to moderate Democrats. Majority leader Harry Reid focused on satisfying centrists. The holdouts came down to Joe Lieberman of Connecticut, an independent who caucused with Democrats, and conservative Nebraska Democrat Ben Nelson. Lieberman's demand that the bill not include a public option[163][180] was met,[181] although supporters won various concessions, including allowing state-based public options such as Vermont's Green Mountain Care.[181][182]
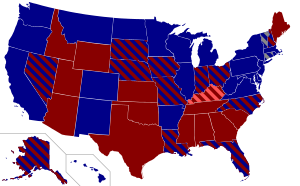
Senate vote by state.
Democratic yes (58)
Independent yes (2)
Republican no (39)
Republican not voting (1)
The White House and Reid addressed Nelson's concerns[183] during a 13-hour negotiation with two concessions: a compromise on abortion, modifying the language of the bill "to give states the right to prohibit coverage of abortion within their own insurance exchanges", which would require consumers to pay for the procedure out of pocket if the state so decided; and an amendment to offer a higher rate of Medicaid reimbursement for Nebraska.[157][184] The latter half of the compromise was derisively termed the "Cornhusker Kickback"[185] and was repealed in the subsequent reconciliation amendment bill.
On December 23, the Senate voted 60–39 to end debate on the bill: a cloture vote to end the filibuster.[186] The bill then passed, also 60–39, on December 24, 2009, with all Democrats and two independents voting for it, and all Republicans against (except Jim Bunning, who did not vote).[187] The bill was endorsed by the AMA and AARP.[188]
On January 19, 2010, Massachusetts Republican Scott Brown was elected to the Senate in a special election to replace Kennedy, having campaigned on giving the Republican minority the 41st vote needed to sustain Republican filibusters.[157][189][190] His victory had become significant because of its effects on the legislative process. The first was psychological: the symbolic importance of losing Kennedy's traditionally Democratic Massachusetts seat made many Congressional Democrats concerned about the political cost of passing a bill.[191][192]
House

House vote by congressional district.
Democratic yes (219)
Democratic no (34)
Republican no (178)
No representative seated (4)
Brown's election meant Democrats could no longer break a filibuster in the Senate. In response, White House Chief of Staff Rahm Emanuel argued that Democrats should scale back to a less ambitious bill; House Speaker Nancy Pelosi pushed back, dismissing Emanuel's scaled-down approach as "Kiddie Care".[193][194]
Obama remained insistent on comprehensive reform. The news that Anthem Blue Cross in California intended to raise premium rates for its patients by as much as 39% gave him new evidence of the need for reform.[193][194] On February 22, he laid out a "Senate-leaning" proposal to consolidate the bills.[195] He held a meeting with both parties' leaders on February 25. The Democrats decided that the House would pass the Senate's bill, to avoid another Senate vote.
House Democrats had expected to be able to negotiate changes in a House–Senate conference before passing a final bill. Since any bill that emerged from conference that differed from the Senate bill would have to pass the Senate over another Republican filibuster, most House Democrats agreed to pass the Senate bill on condition that it be amended by a subsequent bill.[192] They drafted the Health Care and Education Reconciliation Act, which could be passed by the reconciliation process.[193][196][197]
Per the Congressional Budget Act of 1974, reconciliation cannot be subject to a filibuster. But reconciliation is limited to budget changes, which is why the procedure was not used to pass ACA in the first place; the bill had inherently non-budgetary regulations.[198][199] Although the already-passed Senate bill could not have been passed by reconciliation, most of House Democrats' demands were budgetary: "these changes—higher subsidy levels, different kinds of taxes to pay for them, nixing the Nebraska Medicaid deal—mainly involve taxes and spending. In other words, they're exactly the kinds of policies that are well-suited for reconciliation."[196]
The remaining obstacle was a pivotal group of pro-life Democrats led by Bart Stupak who were initially reluctant to support the bill. The group found the possibility of federal funding for abortion significant enough to warrant opposition. The Senate bill had not included language that satisfied their concerns, but they could not address abortion in the reconciliation bill as it would be non-budgetary. Instead, Obama issued Executive Order 13535, reaffirming the principles in the Hyde Amendment.[200] This won the support of Stupak and members of his group and assured the bill's passage.[197][201] The House passed the Senate bill with a 219–212 vote on March 21, 2010, with 34 Democrats and all 178 Republicans voting against it.[202] The next day, Republicans introduced legislation to repeal the bill.[203] Obama signed ACA into law on March 23, 2010.[204] Since passage, Republicans have voted to repeal all or parts of the Affordable Care Act over sixty times; no such attempt by Republicans has been successful.[205] The amendment bill, The Health Care and Education Reconciliation Act, cleared the House on March 21; the Senate passed it by reconciliation on March 25, and Obama signed it on March 30.
Impact
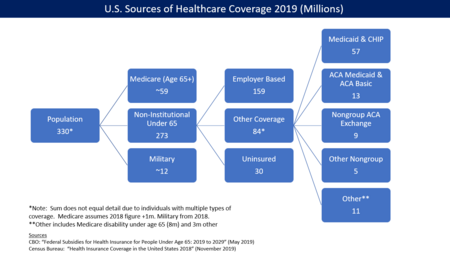
U.S. health insurance coverage by source in 2016. CBO estimated ACA/Obamacare was responsible for 23 million persons covered via exchanges and Medicaid expansion.[6]
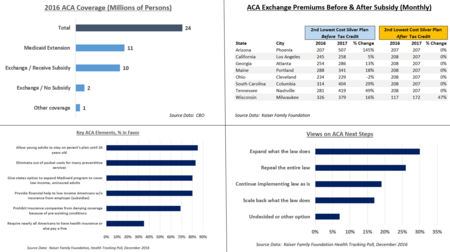
This chart illustrates several aspects of the Affordable Care Act, including number of persons covered, cost before and after subsidies, and public opinion.
Coverage
The law has caused a significant reduction in the number and percentage of people without health insurance. The CDC reported that the percentage of people without health insurance fell from 16.0% in 2010 to 8.9% from January to June 2016.[206] The uninsured rate dropped in every congressional district in the U.S. from 2013 to 2015.[207] The Congressional Budget Office reported in March 2016 that there were approximately 12 million people covered by the exchanges (10 million of whom received subsidies to help pay for insurance) and 11 million made eligible for Medicaid by the law, a subtotal of 23 million people. An additional 1 million were covered by the ACA's "Basic Health Program," for a total of 24 million.[6] CBO also estimated that the ACA would reduce the net number of uninsured by 22 million in 2016, using a slightly different computation for the above figures totaling ACA coverage of 26 million, less 4 million for reductions in "employment-based coverage" and "non-group and other coverage."[6]
The U.S. Department of Health and Human Services (HHS) estimated that 20.0 million adults (aged 18–64) gained healthcare coverage via ACA as of February 2016, a 2.4 million increase over September 2015. HHS estimated that this 20.0 million included: a) 17.7 million from the start of open enrollment in 2013–2016; and b) 2.3 million young adults aged 19–25 who initially gained insurance from 2010 to 2013, as they were allowed to remain on their parent's plans until age 26. Of the 20.0 million, an estimated 6.1 million were aged 19–25.[7] Similarly, the Urban Institute issued a report in December 2016 that said that about 19.2 million non-elderly Americans had gained health insurance coverage from 2010 to 2015.[208] In March 2016, the CBO reported that there were approximately 27 million people without insurance in 2016, a figure they expected would range from 26 to 28 million through 2026. CBO also estimated the percentage of insured among all U.S. residents would remain at 90% during that period, 92–93% excluding unauthorized immigrants.[6]
States that expanded Medicaid had a 7.3% uninsured rate on average in the first quarter of 2016, while those that did not expand it had a 14.1% uninsured rate, among adults aged 18–64.[209] As of December 2016 there were 32 states (including Washington DC) that had adopted the Medicaid extension, while 19 states had not.[210]
By 2017, nearly 70% of those on the exchanges could purchase insurance for less than $75 per month after subsidies, which rose to offset significant pre-subsidy price increases in the exchange markets.[211] Healthcare premium cost increases in the employer market continued to lessen. For example, healthcare premiums for those covered by employers rose by 69% from 2000 to 2005, but only 27% from 2010 to 2015,[11] with only a 3% increase from 2015 to 2016.[212]
The ACA also helps reduce income inequality measured after taxes, due to higher taxes on the top 5% of income earners and both subsidies and Medicaid expansion for lower-income persons.[213] The CBO estimated that subsidies paid under the law in 2016 averaged $4,240 per person for 10 million individuals receiving them, roughly $42 billion. For scale, the subsidy for the employer market, in the form of exempting from taxation those health insurance premiums paid on behalf of employees by employers, was approximately $1,700 per person in 2016, or $266 billion total in the employer market. The employer market subsidy was not changed by the law.[6]
Taxes
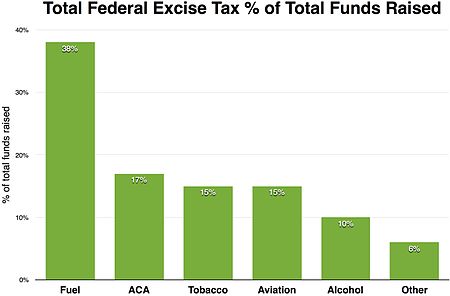
Excise taxes for the Affordable Care Act raised $16.3 billion in fiscal year 2015. $11.3 billion was an excise tax placed directly on health insurers based on their market share. The ACA was going to impose a 40% "Cadillac tax" on expensive employer sponsored health insurance but that was postponed until 2018.[214] Annual excise taxes totaling $3 billion were levied on importers and manufacturers of prescription drugs. An excise tax of 2.32% on medical devices and a 10% excise tax on indoor tanning services were applied as well. The Individual mandate was $695 per individual or $2,085 per family minimum who wasn’t insured and was as high as 2.5% of household income (whichever was higher). The individual mandate was repealed by Republicans ending at the end of 2018.[215] 0.9 percent payroll tax and a 3.8 percent tax on net investment income for individuals with incomes exceeding $200,000 and couples with incomes exceeding $250,000.[216][217]
Insurance exchanges
As of August 2016, 15 states operated their own exchanges. Other states either used the federal exchange, or operated in partnership with or supported by the federal government.[218]
Medicaid expansion

Medicaid expansion by state, as of June 1, 2018.[219]
Adopted the Medicaid expansion
Medicaid expansion under discussion
Not adopting Medicaid expansion
As of December 2016 there were 32 states (including Washington DC) that had adopted the Medicaid extension, while 19 states had not.[210] Those states that expanded Medicaid had a 7.3% uninsured rate on average in the first quarter of 2016, while those that did not expand Medicaid had a 14.1% uninsured rate, among adults aged 18 to 64.[209] Following the Supreme Court ruling in 2012, which held that states would not lose Medicaid funding if they didn't expand Medicaid under the ACA, several states rejected expanded Medicaid coverage. Over half of the national uninsured population lived in those states.[220] In a report to Congress, the Centers for Medicare and Medicaid Services (CMS) estimated that the cost of expansion was $6,366 per person for 2015, about 49 percent above previous estimates. An estimated 9 million to 10 million people had gained Medicaid coverage, mostly low-income adults.[221] The Kaiser Family Foundation estimated in October 2015 that 3.1 million additional people were not covered because of states that rejected the Medicaid expansion.[222]
States that rejected the Medicaid expansion could maintain their Medicaid eligibility thresholds, which in many states were significantly below 133% of the poverty line.[223] Many states did not make Medicaid available to childless adults at any income level.[224] Because subsidies on exchange insurance plans were not available to those below the poverty line, such individuals had no new options.[225][226] For example, in Kansas, where only able-bodied adults with children and with an income below 32% of the poverty line were eligible for Medicaid, those with incomes from 32% to 100% of the poverty level ($6,250 to $19,530 for a family of three) were ineligible for both Medicaid and federal subsidies to buy insurance. Absent children, able-bodied adults were not eligible for Medicaid in Kansas.[220]
Studies of the impact of state decisions to reject the Medicaid expansion calculated that up to 6.4 million people could fall into this status.[227] The federal government initially paid for 100% of the expansion (through 2016). The subsidy tapered to 90% by 2020 and continued to shrink thereafter.[228] Several states argued that they could not afford their 10% contribution.[228][229] Studies suggested that rejecting the expansion would cost more than expanding Medicaid due to increased spending on uncompensated emergency care that otherwise would have been partially paid for by Medicaid coverage,[230]
A 2016 study led by Harvard University health economics professor Benjamin Sommers found that residents of Kentucky and Arkansas, which both accepted the Medicaid expansion, were more likely to receive health care services and less likely to incur emergency room costs or have trouble paying their medical bills than before the expansion. Residents of Texas, which did not accept the Medicaid expansion, did not see a similar improvement during the same period.[231] Kentucky opted for increased managed care, while Arkansas subsidized private insurance. The new Arkansas and Kentucky governors have proposed reducing or modifying their programs. From 2013 to 2015, the uninsured rate dropped from 42% to 14% in Arkansas and from 40% to 9% in Kentucky, compared with 39% to 32% in Texas. Specific improvements included additional primary and preventive care, fewer emergency departments visits, reported higher quality care, improved health, improved drug affordability, reduced out-of-pocket spending and increased outpatient visits, increased diabetes screening, glucose testing among diabetes patients and regular care for chronic conditions.[232]
A 2016 DHHS study found that states that expanded Medicaid had lower premiums on exchange policies, because they had fewer low-income enrollees, whose health on average is worse than that of those with higher income.[233]
Healthcare insurance costs
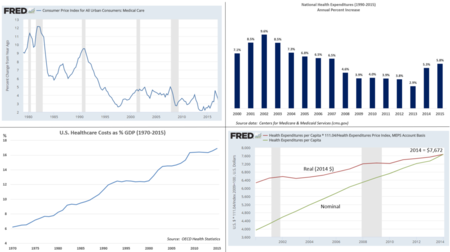
U.S. healthcare cost information, including rate of change, per-capita, and percent of GDP. (Data source: Centers for Medicare and Medicaid Services[234])
The law is designed to pay subsidies in the form of tax credits to the individuals or families purchasing the insurance, based on income levels. Higher income consumers receive lower subsidies. While pre-subsidy prices rose considerably from 2016 to 2017, so did the subsidies, to reduce the after-subsidy cost to the consumer. For example, a study published in 2016 found that the average requested 2017 premium increase among 40-year-old non-smokers was about 9 percent, according to an analysis of 17 cities, although Blue Cross Blue Shield proposed increases of 40 percent in Alabama and 60 percent in Texas.[235] However, some or all of these costs are offset by subsidies, paid as tax credits. For example, the Kaiser Foundation reported that for the second-lowest cost "Silver plan" (a plan often selected and used as the benchmark for determining financial assistance), a 40-year old non-smoker making $30,000 per year would pay effectively the same amount in 2017 as they did in 2016 (about $208/month) after the subsidy/tax credit, despite large increases in the pre-subsidy price. This was consistent nationally. In other words, the subsidies increased along with the pre-subsidy price, fully offsetting the price increases.[236]
Healthcare premium cost increases in the employer market continued to moderate after the implementation of the law. For example, healthcare premiums for those covered by employers rose by 69% from 2000 to 2005, but only 27% from 2010 to 2015,[11] with only a 3% increase from 2015 to 2016.[212] From 2008 to 2010 (before passage of the ACA) health insurance premiums rose by an average of 10% per year.[237]
Several studies found that the financial crisis and accompanying recession could not account for the entirety of the slowdown and that structural changes likely share at least partial credit.[238][239][240][241] A 2013 study estimated that changes to the health system had been responsible for about a quarter of the recent reduction in inflation.[242] Paul Krawzak claimed that even if cost controls succeed in reducing the amount spent on healthcare, such efforts on their own may be insufficient to outweigh the long-term burden placed by demographic changes, particularly the growth of the population on Medicare.[243]
In a 2016 review of the ACA published in JAMA, Barack Obama himself wrote that from 2010 through 2014 mean annual growth in real per-enrollee Medicare spending was negative, down from a mean of 4.7% per year from 2000 through 2005 and 2.4% per year from 2006 to 2010; similarly, mean real per-enrollee growth in private insurance spending was 1.1% per year over the period, compared with a mean of 6.5% from 2000 through 2005 and 3.4% from 2005 to 2010.[244]
Effect on deductibles and co-payments
While health insurance premium costs have moderated, some of this is because of insurance policies that have a higher deductible, co-payments and out-of-pocket maximums that shift costs from insurers to patients. In addition, many employees are choosing to combine a health savings account with higher deductible plans, making the impact of the ACA difficult to determine precisely.
For those who obtain their insurance through their employer ("group market"), a 2016 survey found that:
- Deductibles grew by 63% from 2011 to 2016, while premiums increased 19% and worker earnings grew by 11%.
- In 2016, 4 in 5 workers had an insurance deductible, which averaged $1,478. For firms with less than 200 employees, the deductible averaged $2,069.
- The percentage of workers with a deductible of at least $1,000 grew from 10% in 2006 to 51% in 2016. The 2016 figure drops to 38% after taking employer contributions into account.[245]
For the "non-group" market, of which two-thirds are covered by the ACA exchanges, a survey of 2015 data found that:
- 49% had individual deductibles of at least $1,500 ($3,000 for family), up from 36% in 2014.
- Many marketplace enrollees qualify for cost-sharing subsidies that reduce their net deductible.
- While about 75% of enrollees were "very satisfied" or "somewhat satisfied" with their choice of doctors and hospitals, only 50% had such satisfaction with their annual deductible.
- While 52% of those covered by the ACA exchanges felt "well protected" by their insurance, in the group market 63% felt that way.[246]
Health outcomes
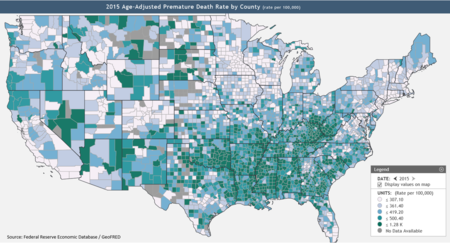
The map illustrates the frequency of premature deaths (those under age 75) adjusted for the age of persons in the county.[247]
Insurance coverage helps save lives, by encouraging early detection and prevention of dangerous medical conditions. According to a 2014 study, the ACA likely prevented an estimated 50,000 preventable patient deaths from 2010 to 2013.[248]City University public health professors David Himmelstein and Steffie Woolhandler wrote in January 2017 that a rollback of the ACA's Medicaid expansion alone would cause an estimated 43,956 deaths annually.[249]
The Federal Reserve publishes data on premature death rates by county, defined as those dying below age 74.[247] According to the Kaiser Foundation, expanding Medicaid in the remaining 19 states would cover up to 4.5 million persons.[250] Since expanding Medicaid expands coverage[250] and expanding coverage reduces mortality,[248] therefore expanding Medicaid reduces mortality by syllogism. Texas, Oklahoma, Mississippi, Alabama, Georgia, Tennessee, Missouri and South Carolina, indicated on the map at right as having many counties with high premature mortality rates[247] could therefore reduce mortality by expanding Medicaid, other things equal.
Distributional impact

The distributional impact of the Affordable Care Act (ACA or Obamacare) during 2014. The ACA raised taxes mainly on the top 1% to fund approximately $600 in benefits on average for the bottom 40% of families.
In March 2018, the CBO reported that the ACA had reduced income inequality in 2014, saying that the law led the lowest and second quintiles (the bottom 40%) to receive an average of an additional $690 and $560 respectively while causing households in the top 1% to pay an additional $21,000 due mostly to the net investment income tax and the additional Medicare tax. The law placed relatively little burden on households in the top quintile (top 20%) outside of the top 1%.[10]
Federal deficit
CBO estimates of revenue and impact on deficit
The CBO reported in several studies that the ACA would reduce the deficit, and that repealing it would increase the deficit.[8][9][251][252] The 2011 comprehensive CBO estimate projected a net deficit reduction of more than $200 billion during the 2012–2021 period:[9][253] it calculated the law would result in $604 billion in total outlays offset by $813 billion in total receipts, resulting in a $210 billion net deficit reduction.[9] The CBO separately predicted that while most of the spending provisions do not begin until 2014,[254][255] revenue would exceed spending in those subsequent years.[256] The CBO claimed that the bill would "substantially reduce the growth of Medicare's payment rates for most services; impose an excise tax on insurance plans with relatively high premiums; and make various other changes to the federal tax code, Medicare, Medicaid, and other programs"[257]—ultimately extending the solvency of the Medicare trust fund by 8 years.[258]
This estimate was made prior to the Supreme Court's ruling that enabled states to opt out of the Medicaid expansion, thereby forgoing the related federal funding. The CBO and JCT subsequently updated the budget projection, estimating the impact of the ruling would reduce the cost estimate of the insurance coverage provisions by $84 billion.[259][260][261]
The CBO in June 2015 forecast that repeal of ACA would increase the deficit between $137 billion and $353 billion over the 2016–2025 period, depending on the impact of macroeconomic feedback effects. The CBO also forecasted that repeal of ACA would likely cause an increase in GDP by an average of 0.7% in the period from 2021 to 2025, mainly by boosting the supply of labor.[8]
Although the CBO generally does not provide cost estimates beyond the 10-year budget projection period because of the degree of uncertainty involved in the projection, it decided to do so in this case at the request of lawmakers, and estimated a second decade deficit reduction of $1.2 trillion.[257][262] CBO predicted deficit reduction around a broad range of one-half percent of GDP over the 2020s while cautioning that "a wide range of changes could occur".[263]
Opinions on CBO projections
The CBO cost estimates were criticized because they excluded the effects of potential legislation that would increase Medicare payments by more than $200 billion from 2010 to 2019.[264][265][266] However, the so-called "doc fix" is a separate issue that would have existed whether or not ACA became law – omitting its cost from ACA was no different from omitting the cost of other tax cuts.[267][268][269]
Uwe Reinhardt, a Princeton health economist, wrote. "The rigid, artificial rules under which the Congressional Budget Office must score proposed legislation unfortunately cannot produce the best unbiased forecasts of the likely fiscal impact of any legislation", but went on to say "But even if the budget office errs significantly in its conclusion that the bill would actually help reduce the future federal deficit, I doubt that the financing of this bill will be anywhere near as fiscally irresponsible as was the financing of the Medicare Modernization Act of 2003."[270]Douglas Holtz-Eakin, CBO director during the George W. Bush administration, who later served as the chief economic policy adviser to U.S. Senator John McCain's 2008 presidential campaign, alleged that the bill would increase the deficit by $562 billion because, he argued, it front-loaded revenue and back-loaded benefits.[271]
Scheiber and Cohn rejected critical assessments of the law's deficit impact, arguing that predictions were biased towards underestimating deficit reduction. They noted that for example, it is easier to account for the cost of definite levels of subsidies to specified numbers of people than account for savings from preventive healthcare, and that the CBO had a track record of overestimating costs and underestimating savings of health legislation;[272][273] stating, "innovations in the delivery of medical care, like greater use of electronic medical records[274] and financial incentives for more coordination of care among doctors, would produce substantial savings while also slowing the relentless climb of medical expenses... But the CBO would not consider such savings in its calculations, because the innovations hadn't really been tried on such large scale or in concert with one another—and that meant there wasn't much hard data to prove the savings would materialize."[272]
In 2010, David Walker, former U.S. Comptroller General then working for The Peter G. Peterson Foundation, stated that the CBO estimates are not likely to be accurate, because they were based on the assumption that the law would not change.[275] The Center on Budget and Policy Priorities objected that Congress had a good record of implementing Medicare savings. According to their study, Congress followed through on the implementation of the vast majority of provisions enacted in the past 20 years to produce Medicare savings, although not the payment reductions addressed by the annual "doc fix".[276][277]
Economic consequences

Coverage rate, employer market cost trends, budgetary impact, and income inequality aspects of the Affordable Care Act.
CBO estimated in June 2015 that repealing the ACA would:
- Decrease aggregate demand (GDP) in the short-term, as low-income persons who tend to spend a large fraction of their additional resources would have fewer resources (e.g., ACA subsidies would be eliminated). This effect would be offset in the long-run by the labor supply factors below.
- Increase the supply of labor and aggregate compensation by about 0.8 and 0.9 percent over the 2021–2025 period. CBO cited the ACA's expanded eligibility for Medicaid and subsidies and tax credits that rise with income as disincentives to work, so repealing the ACA would remove those disincentives, encouraging workers to supply more hours of labor.
- Increase the total number of hours worked by about 1.5% over the 2021–2025 period.
- Remove the higher tax rates on capital income, thereby encouraging additional investment, raising the capital stock and output in the long-run.[8]
In 2015 the Center for Economic and Policy Research found no evidence that companies were reducing worker hours to avoid ACA requirements[278] for employees working over 30 hours per week.[279]
The CBO estimated that the ACA would slightly reduce the size of the labor force and number of hours worked, as some would no longer be tethered to employers for their insurance. Cohn, citing CBO's projections, claimed that ACA's primary employment effect was to alleviate job lock: "People who are only working because they desperately need employer-sponsored health insurance will no longer do so."[280] He concluded that the "reform's only significant employment impact was a reduction in the labor force, primarily because people holding onto jobs just to keep insurance could finally retire", because they have health insurance outside of their jobs.[281]
Employer mandate and part-time work
The employer mandate requires employers meeting certain criteria to provide health insurance to their workers. The mandate applies to employers with more than 50 employees that do not offer health insurance to their full-time workers.[282] Critics claimed that the mandate created a perverse incentive for business to keep their full-time headcount below 50 and to hire part-time workers instead.[283][284] Between March 2010 and 2014 the number of part-time jobs declined by 230,000, while the number of full-time jobs increased by 2 million.[285][286] In the public sector full-time jobs turned into part-time jobs much more than in the private sector.[285][287] A 2016 study found only limited evidence that ACA had increased part-time employment.[288]
Several businesses and the state of Virginia added a 29-hour-a-week cap for their part-time employees,[289][unreliable source?][290][unreliable source?] to reflect the 30-hour-or-more definition for full-time worker.[282] As of yet, however, only a small percent of companies have shifted their workforce towards more part-time hours (4% in a survey from the Federal Reserve Bank of Minneapolis).[284] Trends in working hours[291] and the effects of the Great Recession correlate with part-time working hour patterns.[292][293] The impact of this provision may have been offset by other factors, including that health insurance helps attract and retain employees, increases productivity and reduces absenteeism; and the lower training and administration costs of a smaller full-time workforce over a larger part-time work force.[284][291][294] Relatively few firms employ over 50 employees[284] and more than 90% of them offered insurance.[295] Workers without employer insurance could purchase insurance on the exchanges.[296]
Most policy analysts (on both right and left) were critical of the employer mandate provision.[283][295] They argued that the perverse incentives regarding part-time hours, even if they did not change existing plans, were real and harmful;[297][298] that the raised marginal cost of the 50th worker for businesses could limit companies' growth;[299] that the costs of reporting and administration were not worth the costs of maintaining employer plans;[297][298] and noted that the employer mandate was not essential to maintain adequate risk pools.[300][301] The effects of the provision generated vocal opposition from business interests and some unions not granted exemptions.[298][302]
A 2013/4 survey by the National Association for Business Economics found that about 75 percent of those surveyed said ACA hadn't influenced their planning or expectations for 2014, and 85 percent said the law wouldn't prompt a change in their hiring practices. Some 21 percent of 64 businesses surveyed said that the act would have a harmful effect and 5 percent said it would be beneficial.[303]
Hospitals
From the start of 2010 to November 2014, 43 hospitals in rural areas closed. Critics claimed that the new law caused these hospitals to close. Many of these rural hospitals were built using funds from the 1946 Hill–Burton Act, to increase access to medical care in rural areas. Some of these hospitals reopened as other medical facilities, but only a small number operated emergency rooms (ER) or urgent care centers.[304]
Between January 2010 and 2015, a quarter of emergency room doctors said they had seen a major surge in patients, while nearly half had seen a smaller increase. Seven in ten ER doctors claimed that they lacked the resources to deal with large increases in the number of patients. The biggest factor in the increased number of ER patients was insufficient primary care providers to handle the larger number of insured patients.[305]
Insurers claimed that because they have access to and collect patient data that allow evaluations of interventions, they are essential to ACO success. Large insurers formed their own ACOs. Many hospitals merged and purchased physician practices. The increased market share gave them more leverage in negotiations with insurers over costs and reduced patient care options.[118]
Public opinion
Prior to the law's passage, polling indicated the public's views became increasingly negative in reaction to specific plans discussed during the legislative debate over 2009 and 2010. Polling statistics showed a general negative opinion of the law; with those in favor at approximately 40% and those against at 51%, as of October 2013.[306][307] About 29% of whites approve of the law, compared with 61% of Hispanics and 91% of African Americans.[308] Opinions were divided by age of the person at the law's inception, with a solid majority of seniors opposing the bill and a solid majority of those younger than forty years old in favor.[309]

Congressional Democrats celebrating the 6th anniversary of the Affordable Care Act in March 2016 on the steps of the U.S. Capitol.
Specific elements were popular across the political spectrum, while others, such as the mandate to purchase insurance, were widely disliked. In a 2012 poll 44% supported the law, with 56% against. By party affiliation, 75% of Democrats, 27% of Independents and 14% of Republicans favored the law overall. 82% favored banning insurance companies from denying coverage to people with pre-existing conditions, 61% favored allowing children to stay on their parents' insurance until age 26, 72% supported requiring companies with more than 50 employees to provide insurance for their employees, and 39% supported the individual mandate to own insurance or pay a penalty. By party affiliation, 19% of Republicans, 27% of Independents, and 59% of Democrats favored the mandate.[310] Other polls showed additional provisions receiving majority support, including the creation of insurance exchanges, pooling small businesses and the uninsured with other consumers so that more people can take advantage of large group pricing benefits and providing subsidies to individuals and families to make health insurance more affordable.[311][312]
In a 2010 poll, 62% of respondents said they thought ACA would "increase the amount of money they personally spend on health care", 56% said the bill "gives the government too much involvement in health care", and 19% said they thought they and their families would be better off with the legislation.[313] Other polls found that people were concerned that the law would cost more than projected and would not do enough to control costs.[314]
Some opponents believed that the reform did not go far enough: a 2012 poll indicated that 71% of Republican opponents rejected it overall, while 29% believed it did not go far enough; independent opponents were divided 67% to 33%; and among the much smaller group of Democratic opponents, 49% rejected it overall and 51% wanted more.[310]
In June 2013, a majority of the public (52–34%) indicated a desire for "Congress to implement or tinker with the law rather than repeal it".[315] After the Supreme Court upheld the individual mandate, a 2012 poll held that "most Americans (56%) want to see critics of President Obama's health care law drop efforts to block it and move on to other national issues".[316]A 2014 poll reported that 48.9% of respondents had an unfavorable view of ACA vs. 38.3% who had a favorable view (of more than 5,500 individuals).[317]
A 2014 poll reported that 26% of Americans support ACA.[318] Another held that 8% of respondents say that the Affordable Care Act "is working well the way it is".[319] In late 2014, a Rasmussen poll reported Repeal: 30%, Leave as is: 13%, Improve: 52%.[320]
In 2015, a CBS News / New York Times poll reported that 47% of Americans approved the health care law. This was the first time that a major poll indicated that more respondents approved ACA than disapproved of it.[321] The recurring Kaiser Health Tracking Poll from December 2016 reported that: a) 30% wanted to expand what the law does; b) 26% wanted to repeal the entire law; c) 19% wanted to move forward with implementing the law as it is; and d) 17% wanted to scale back what the law does, with the remainder undecided.[322]
Separate polls from Fox News and NBC/WSJ both taken during January 2017 indicated more people viewed the law favorably than did not for the first time. One of the reasons for the improving popularity of the law is that Democrats who opposed it in the past (many prefer a "Medicare for All" approach) have shifted their positions since the ACA is under threat of repeal.[323]
A January 2017 Morning Consult poll showed that 35% of respondents either believed that "Obamacare" and the "Affordable Care Act" were different or did not know.[324] Approximately 45% were unsure whether the "repeal of Obamacare" also meant the "repeal of the Affordable Care Act."[324] 39% did not know that "many people would lose coverage through Medicaid or subsidies for private health insurance if the A.C.A. were repealed and no replacement enacted," with Democrats far more likely (79%) to know that fact than Republicans (47%).[324]
A 2017 study found that personal experience with public health insurance programs leads to greater support for the Affordable Care Act, and the effects appear to be most pronounced among Republicans and low-information voters.[325]
Political aspects
"Obamacare"
The term "Obamacare" was originally coined by opponents as a pejorative. The term emerged in March 2007 when healthcare lobbyist Jeanne Schulte Scott used it in a health industry journal, writing "We will soon see a 'Giuliani-care' and 'Obama-care' to go along with 'McCain-care', 'Edwards-care', and a totally revamped and remodeled 'Hillary-care' from the 1990s".[1][326] According to research by Elspeth Reeve, the expression was used in early 2007, generally by writers describing the candidate's proposal for expanding coverage for the uninsured.[327] It first appeared in a political campaign by Mitt Romney in May 2007 in Des Moines, Iowa. Romney said, "In my state, I worked on healthcare for some time. We had half a million people without insurance, and I said, 'How can we get those people insured without raising taxes and without having government take over healthcare?' And let me tell you, if we don't do it, the Democrats will. If the Democrats do it, it will be socialized medicine; it'll be government-managed care. It'll be what's known as Hillarycare or Barack Obamacare, or whatever you want to call it."[1]
By mid-2012, Obamacare had become the colloquial term used by both supporters and opponents. In contrast, the use of "Patient Protection and Affordable Care Act" or "Affordable Care Act" became limited to more formal and official use.[327] Use of the term in a positive sense was suggested by Democrat John Conyers.[328] Obama endorsed the nickname, saying, "I have no problem with people saying Obama cares. I do care."[329]
In March 2012, the Obama reelection campaign embraced the term "Obamacare", urging Obama's supporters to post Twitter messages that begin, "I like #Obamacare because...".[330]
In October 2013, the Associated Press and NPR began cutting back on use of the term.[331] Stuart Seidel, NPR's managing editor, said that the term "seems to be straddling somewhere between being a politically-charged term and an accepted part of the vernacular".[332]
Common misconceptions
"Death panels"
On August 7, 2009, Sarah Palin pioneered the term "death panels" to describe groups that would decide whether sick patients were "worthy" of medical care.[333]
"Death panel" referred to two claims about early drafts.
One was that under the law, seniors could be denied care due to their age[334] and the other that the government would advise seniors to end their lives instead of receiving care. The ostensible basis of these claims was the provision for an Independent Payment Advisory Board (IPAB).[335] IPAB was given the authority to recommend cost-saving changes to Medicare by facilitating the adoption of cost-effective treatments and cost-recovering measures when the statutory levels set for Medicare were exceeded within any given 3-year period. In fact, the Board was prohibited from recommending changes that would reduce payments to certain providers before 2020, and was prohibited from recommending changes in premiums, benefits, eligibility and taxes, or other changes that would result in rationing.[336][337]
The other related issue concerned advance-care planning consultation: a section of the House reform proposal would have reimbursed physicians for providing patient-requested consultations for Medicare recipients on end-of-life health planning (which is covered by many private plans), enabling patients to specify, on request, the kind of care they wished to receive.[338] The provision was not included in ACA.[339]
In 2010, the Pew Research Center reported that 85% of Americans were familiar with the claim, and 30% believed it was true, backed by three contemporaneous polls.[340] A poll in August 2012 found that 39% of Americans believed the claim.[341]
The allegation was named PolitiFact's "Lie of the Year",[333][342] one of FactCheck.org's "whoppers"[343][344] and the most outrageous term by the American Dialect Society.[345]AARP described such rumors as "rife with gross—and even cruel—distortions".[346]
Members of Congress
ACA requires members of Congress and their staffs to obtain health insurance either through an exchange or some other program approved by the law (such as Medicare), instead of using the insurance offered to federal employees (the Federal Employees Health Benefits Program).[347][348][349][350][351]
Illegal immigrants
ACA does not provide benefits to illegal immigrants.[352] It explicitly denies insurance subsidies to "unauthorized (illegal) aliens".[65][66][353]
Exchange "death spiral"
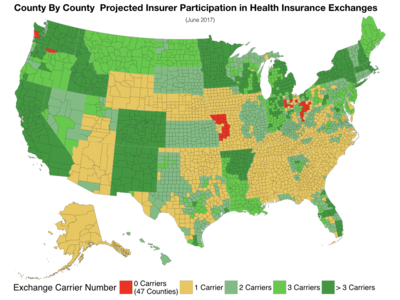
One argument against the ACA is that the insurers are leaving the marketplaces, as they cannot profitably cover the available pool of customers, which contains too many unhealthy participants relative to healthy participants. A scenario where prices rise, due to an unfavorable mix of customers from the insurer's perspective, resulting in fewer customers and fewer insurers in the marketplace, further raising prices, has been called a "death spiral."[354] During 2017, the median number of insurers offering plans on the ACA exchanges in each state was 3.0, meaning half the states had more and half had fewer insurers. There were five states with one insurer in 2017; 13 states with two; 11 states with three; and the remainder had four insurers or more. Wisconsin had the most, with 15 insurers in the marketplace. The median number of insurers was 4.0 in 2016, 5.0 in 2015, and 4.0 in 2014.[355]
Further, the CBO reported in January 2017 that it expected enrollment in the exchanges to rise from 10 million during 2017 to 13 million by 2027, assuming laws in place at the end of the Obama administration were continued.[356] Following a 2015 CBO report that reached a similar conclusion, Paul Krugman wrote: "But the truth is that this report is much, much closer to what supporters of reform have said than it is to the scare stories of the critics—no death spirals, no job-killing, major gains in coverage at relatively low cost."[357]
Opposition
Opposition and efforts to repeal the legislation have drawn support from sources that include labor unions,[358][359]conservative advocacy groups,[360][361] Republicans, small business organizations and the Tea Party movement.[362] These groups claimed that the law would disrupt existing health plans, increase costs from new insurance standards, and increase the deficit.[363] Some opposed the idea of universal healthcare, viewing insurance as similar to other unsubsidized goods.[364][365] President Donald Trump has repeatedly promised to "repeal and replace" it.[366][367]
As of 2013[update] unions that expressed concerns about ACA included the AFL-CIO,[368] which called ACA "highly disruptive" to union health care plans, claiming it would drive up costs of union-sponsored plans; the International Brotherhood of Teamsters, United Food and Commercial Workers International Union, and UNITE-HERE, whose leaders sent a letter to Reid and Pelosi arguing, " ACA will shatter not only our hard-earned health benefits, but destroy the foundation of the 40-hour work week that is the backbone of the American middle class."[359] In January 2014, Terry O'Sullivan, president of the Laborers' International Union of North America (LIUNA) and D. Taylor, president of Unite Here sent a letter to Reid and Pelosi stating, "ACA, as implemented, undermines fair marketplace competition in the health care industry."[358]
In October 2016, Mark Dayton, the governor of Minnesota and a member of the Minnesota Democratic–Farmer–Labor Party, said that the ACA had "many good features" but that it was "no longer affordable for increasing numbers of people" and called on the Minnesota legislature to provide emergency relief to policyholders.[369] Dayton later said he regretted his remarks after they were seized on by Republicans seeking to repeal the law.[370]
Legal challenges
National Federation of Independent Business v. Sebelius
Opponents challenged ACA's constitutionality in multiple lawsuits on multiple grounds.[371][372][not in citation given] In National Federation of Independent Business v. Sebelius, the Supreme Court ruled on a 5–4 vote that the individual mandate was constitutional when viewed as a tax, although not under the Commerce Clause.
The Court further determined that states could not be forced to participate in the Medicaid expansion. ACA withheld all Medicaid funding from states declining to participate in the expansion. The Court ruled that this withdrawal of funding was unconstitutionally coercive and that individual states had the right to opt out without losing preexisting Medicaid funding.[13]
Contraception mandate
In March 2012, the Roman Catholic Church, while supportive of ACA's objectives, voiced concern through the United States Conference of Catholic Bishops that aspects of the mandate covering contraception and sterilization and HHS's narrow definition of a religious organization violated the First Amendment right to free exercise of religion and conscience. Various lawsuits addressed these concerns.[373][374]
On June 25, 2015, the U.S. Supreme Court ruled 6–3 that federal subsidies for health insurance premiums could be used in the 34 states that did not set up their own insurance exchanges.[375]
House v. Price
In United States House of Representatives v. Price (previously United States House of Representatives v. Burwell) the House sued the administration alleging that the money for premium subsidy payments to insurers had not been appropriated, as required for any federal government spending. The ACA subsidy that helps customers pay premiums was not part of the suit.
Without the cost-sharing subsidies, the government estimated that premiums would increase by 20 percent to 30 percent for silver plans.[376] In 2017, the uncertainty about whether the payments would continue caused Blue Cross Blue Shield of North Carolina to try to raise premiums by 22.9 percent the next year, as opposed to an increase of only 8.8 percent that it would have sought if the payments were assured.[377]
Non-cooperation
Officials in Texas, Florida, Alabama, Wyoming, Arizona, Oklahoma and Missouri opposed those elements of ACA over which they had discretion.[378][379] For example, Missouri declined to expand Medicaid or establish a health insurance marketplace engaging in active non-cooperation, enacting a statute forbidding any state or local official to render any aid not specifically required by federal law.[380] Other Republican politicians discouraged efforts to advertise the benefits of the law. Some conservative political groups launched ad campaigns to discourage enrollment.[381][382]
Repeal efforts
ACA was the subject of unsuccessful repeal efforts by Republicans in the 111th, 112th, and 113th Congresses: Representatives Steve King (R-IA) and Michele Bachmann (R-MN) introduced bills in the House to repeal ACA the day after it was signed, as did Senator Jim DeMint (R-SC) in the Senate.[383] In 2011, after Republicans gained control of the House of Representatives, one of the first votes held was on a bill titled "Repealing the Job-Killing Health Care Law Act" (H.R. 2), which the House passed 245–189.[384] All Republicans and 3 Democrats voted for repeal.[385] House Democrats proposed an amendment that repeal not take effect until a majority of the Senators and Representatives had opted out of the Federal Employees Health Benefits Program; Republicans voted down the measure.[386] In the Senate, the bill was offered as an amendment to an unrelated bill, but was voted down.[387] President Obama had stated that he would have vetoed the bill even if it had passed both chambers of Congress.[388]

2017 House Budget
Following the 2012 Supreme Court ruling upholding ACA as constitutional, Republicans held another vote to repeal the law on July 11;[389] the House of Representatives voted with all 244 Republicans and 5 Democrats in favor of repeal, which marked the 33rd, partial or whole, repeal attempt.[390][391] On February 3, 2015, the House of Representatives added its 67th repeal vote to the record (239 to 186). This attempt also failed.[392]
2013 federal government shutdown
Strong partisan disagreement in Congress prevented adjustments to the Act's provisions.[393] However, at least one change, a proposed repeal of a tax on medical devices, has received bipartisan support.[394] Some Congressional Republicans argued against improvements to the law on the grounds they would weaken the arguments for repeal.[298][395]
Republicans attempted to defund its implementation,[379][396] and in October 2013, House Republicans refused to fund the federal government unless accompanied with a delay in ACA implementation, after the President unilaterally deferred the employer mandate by one year, which critics claimed he had no power to do. The House passed three versions of a bill funding the government while submitting various versions that would repeal or delay ACA, with the last version delaying enforcement of the individual mandate. The Democratic Senate leadership stated the Senate would only pass a "clean" funding bill without any restrictions on ACA. The government shutdown began on October 1.[397][398][399] Senate Republicans threatened to block appointments to relevant agencies, such as the Independent Payment Advisory Board[400] and Centers for Medicare and Medicaid Services.[401][402]
2017 repeal effort
During a midnight congressional session starting January 11, 2017, the Senate of the 115th Congress of the United States voted to approve a "budget blueprint" which would allow Republicans to repeal parts of the law "without threat of a Democratic filibuster."[403][404] The plan, which passed 51–48, is a budget blueprint named by Senate Republicans the "Obamacare 'repeal resolution.'"[405] Democrats opposing the resolution staged a protest during the vote.[406]
House Republicans announced their replacement for the ACA, the American Health Care Act, on March 6, 2017.[407] On March 24, 2017 the effort, led by Paul Ryan and Donald Trump, to repeal and replace the ACA failed amid a revolt among Republican representatives.[408]
May 4, 2017, the United States House of Representatives voted to pass the American Health Care Act (and thereby repeal most of the Affordable Care Act) by a narrow margin of 217 to 213, sending the bill to the Senate for deliberation.[409] The Senate Republican leadership announced that Senate Republicans would write their own version of the bill, instead of voting on the House version.[410]
The Senate process began with an unprecedented level of secrecy; Senate Majority Leader Mitch McConnell named a group of 13 Republican Senators to draft the Senate's substitute version in private, raising bipartisan concerns about a lack of transparency.[411][412][413] On June 22, 2017, Republicans released the first discussion draft for an amendment to the bill, which would rename it to the "Better Care Reconciliation Act of 2017" (BCRA).[414] On July 25, 2017, although no amendment proposal had yet garnered majority support, Senate Republicans voted to advance the bill to the floor and begin formal consideration of amendments. Senators Susan Collins and Lisa Murkowski were the only two dissenting Republicans making the vote a 50–50 tie. Vice President Mike Pence then cast the tiebreaking vote in the affirmative.[415]
All specific bills were defeated, however. The revised BCRA failed on a vote of 43–57. A subsequent "Obamacare Repeal and Reconciliation Act" abandoned the "repeal and replace" approach in favor of a straight repeal, but failed on a vote of 45–55. Finally, the "Health Care Freedom Act", nicknamed "skinny repeal" because it would have made the least change to the ACA, failed by 49–51, with Collins, Murkowski, and Senator John McCain joining all the Democrats and independents in voting against it.[416]
Actions to hinder implementation

Tax Cuts and Jobs Act - Number of additional persons uninsured.[417]
Under both the ACA (current law) and the AHCA, CBO reported that the health exchange marketplaces would remain stable (i.e., no "death spiral").[418] However, Republican politicians have taken a variety of steps to undermine it, creating uncertainty that has adversely impacted enrollment and insurer participation while increasing premiums.[419] Insisting the exchanges are in difficulty was also used as an argument for passing reforms such as AHCA or BCRA. Past and ongoing Republican attempts to weaken the law have included, among others:
- Lawsuits such as King v. Burwell, which resulted in a decision by the Supreme Court that limited Medicaid expansion but upheld the mandates and insurance subsidies. According to the Kaiser Family Foundation, not expanding Medicaid in 19 states has increased the number uninsured by an estimated 4.5 million persons.[420]
- Lawsuits pending (House v. Price) such as whether cost-sharing subsidies must be paid. President Trump threatened not to pay these subsidies in early 2017 and later decided to stop paying them. CBO estimated in September 2017 that discontinuing the payments would add an average of 15–20 percentage points to health insurance costs on the exchanges in 2018 while increasing the budget deficit nearly $200 billion over a decade.[421]
- Prevention of appropriations for transitional financing ("risk corridors") to steady insurance markets, resulting the bankruptcy of many co-ops offering insurance. This action was attributed to Senator Marco Rubio.[422]
- Weakening of the individual mandate through his first executive order, which resulted in limiting enforcement of mandate penalties by the IRS. For example, tax returns without indications of health insurance ("silent returns") will still be processed, overriding instructions from the Obama administration to the IRS to reject them.[423]
- Reduction to funding for advertising for the 2017 and 2018 exchange enrollment periods by up to 90%, with other reductions to support resources used to answer questions and help people sign-up for coverage.[424] CBO said in September 2017 that the reductions would lead to reduced ACA enrollment.[421]
- The Trump administration reduced the enrollment period for 2018 by half, to 45 days. The NYT editorial board referred to this as part of a concerted "sabotage" effort.[425]
- Public statements by Trump that the exchanges are unstable or in a death spiral.[426]
- Trump's October 12, 2017 executive order and a related action the same day ending federal subsidies of questionable legality[427] used to help those buying insurance through exchanges with their co-payments and deductibles. About 6 million people were helped at a cost of $7 billion a year but that amount was expected to double in 10 years. State officials claimed the action caused insurance premiums to go up dramatically. Many states sued in federal court on the grounds that Trump was not legally allowed to take the action.[428]
- Several insurers and actuary groups cited uncertainty created by President Trump, specifically non-enforcement of the individual mandate and not funding cost sharing reduction subsidies, as contributing 20–30 percentage points to premium increases for the 2018 plan year on the ACA exchanges. In other words, absent Trump's actions against the ACA, premium increases would have averaged 10% or less, rather than the estimated 28–40% under the uncertainty his actions created.[429]
- The progressive think tank Center on Budget and Policy Priorities (CBPP) maintains a timeline of many "sabotage" efforts by the Trump Administration.[430]
Ending cost-sharing reduction (CSR) payments
President Trump announced on October 12, 2017[431] he would end the smaller of the two types of subsidies under the ACA, the cost sharing reduction (CSR) subsidies. This controversial decision significantly raised premiums on the ACA exchanges along with the premium tax credit subsidies that rise with them, with the CBO estimating a $200 billion increase in the budget deficit over a decade. The reasons for this are complex and require discussion of how the two major subsidies work.[432]
The CSR subsidies are paid to insurance companies to reduce copayments and deductibles for a smaller group of ACA enrollees, those earning less than 250% of the federal poverty line (FPL). The second and larger type of subsidy, the premium tax credits designed to reduce the post-subsidy cost of monthly premiums, apply to all enrollees earning less than 400% of the FPL. For scale, during 2017, approximately $7 billion in CSR subsidies will be paid, versus $34 billion for the premium tax credits.[433] A court decision meant that CSR subsidies were treated as discretionary spending, meaning Congress must decide to appropriate funds for them each year. This effectively gave the President the power to end them, as Democrats with a minority in Congress could not appropriate the funds, let alone override his veto of an appropriations bill.[432]
However, the premium tax credits are mandatory spending, meaning all those eligible under the ACA receive them without Congressional appropriation. These adjust with premium increases to limit after-subsidy premium payments by ACA enrollees to a fixed percentage of income. Based on President Trump's threats to end the CSR payments during early 2017, several insurers and actuarial groups estimated this resulted in a 20 percentage point or more increase in premiums for the 2018 plan year. In other words, premium increases expected to be 10% or less in 2018 became 28–40% instead.[429][432]
The CBO reported in August 2017 (prior to President Trump's decision) that ending the CSR payments might increase ACA premiums by 20 percentage points or more, with a resulting increase of nearly $200 billion in the budget deficit over a decade, as the premium tax credit subsidies would rise along with premium prices. CBO also estimated that initially up to one million fewer would have health insurance coverage, although more might have it in the long-run as the subsidies expand. CBO expected the exchanges to remain stable (i.e., no "death spiral" before or after Trump's action) as the premiums would increase and prices would stabilize at the higher (non-CSR) level.[434]
CBO estimated that of the 12 million with private insurance via the ACA exchanges in 2017, about 10 million receive premium tax credit subsidies and will be shielded from premium increases, as their after-subsidy premiums are limited as a percentage of income under the ACA. However, those 2 million who do not receive subsidies face the brunt of the 20%+ premium increases, without subsidy assistance. This may adversely impact enrollment in 2018 and beyond. Another 13 million who are covered under the ACA's Medicaid expansion (in the 31 states that chose to expand coverage) should not be directly affected by Trump's action.[434][433]
President Trump's argument that the CSR payments were a "bailout" for insurance companies and therefore should be stopped, actually results in the government paying more to insurance companies ($200B over a decade) due to increases in the premium tax credit subsidies.[432]
Implementation
At various times during and after the ACA debate, Obama stated that "if you like your health care plan, you'll be able to keep your health care plan".[435][436] However, in fall 2013 millions of Americans with individual policies received notices that their insurance plans were terminated,[437] and several million more risked seeing their current plans cancelled.[438][439][440] However, Poltifact cited various estimates that only about 2% of the total insured population (4 million out of 262 million) received such notices.[441] Obama's previous unambiguous assurance that consumers' could keep their own plans became a focal point for critics, who challenged his truthfulness.[442][443] On November 7, 2013, President Obama stated: "I am sorry that [people losing their plans] are finding themselves in this situation based on assurances they got from me."[444] Various bills were introduced in Congress to allow people to keep their plans.[445]
In 2010 small business tax credits took effect.[446] Then Pre-Existing Condition Insurance Plan (PCIP) took effect to offer insurance to those that had been denied coverage by private insurance companies because of a pre-existing condition.[446] By 2011, insurers had stopped marketing child-only policies in 17 states, as they sought to escape this requirement.[447] In National Federation of Independent Business v. Sebelius decided on June 28, 2012, the Supreme Court ruled that the individual mandate was constitutional when the associated penalties were construed as a tax. The decision allowed states to opt out of the Medicaid expansion.[448][449][450]
In 2013, the Internal Revenue Service ruled that the cost of covering only the individual employee would be considered in determining whether the cost of coverage exceeded 9.5% of income. Family plans would not be considered even if the cost was above the 9.5% income threshold.[451][452] In July 2 it was announced the implementation of the employer mandate would be delayed until 2015.[295][453][454] The launch for both the state and federal exchanges was troubled due to management and technical failings. HealthCare.gov, the website that offers insurance through the exchanges operated by the federal government, crashed on opening and suffered endless problems.[455] Operations stabilized in 2014, although not all planned features were complete.[456][457]
The Government Accountability Office released a non-partisan study in 2014 that concluded that the administration did not provide "effective planning or oversight practices" in developing the ACA website.[458] In Burwell v. Hobby Lobby the Supreme Court exempted closely held corporations with religious convictions from the contraception rule.[459] At the beginning of the 2015, 11.7 million had signed up (ex-Medicaid).[460] By the end of the year about 8.8 million consumers had stayed in the program.[461] The December spending bill delayed the onset of the "Cadillac tax" on expensive insurance plans by two years, until 2020.[462]
An estimated 9 million to 10 million people had gained Medicaid coverage in 2016, mostly low-income adults.[221] A survey of New York businesses found an increase of 8.5 percent in health care costs, less than the prior year's survey had expected.[463] The five major national insurers expected to lose money on ACA policies in 2016.[464] One of the causes of insurer losses is the lower income, older and sicker enrollee population.[465] Newly elected Louisiana Governor John Bel Edwards issued an executive order to accept the expansion, becoming the 32nd state to do so. The program was expected to enroll an additional 300,000 Louisianans.[466]
More than 9.2 million people signed up for care on the national exchange (healthcare.gov) for 2017, down some 400,000 from 2016. This decline was due primarily to the election of President Trump.[467] Of the 9.2 million, 3.0 million were new customers and 6.2 million were returning. The 9.2 million excludes the 11 states that run their own exchanges, which have signed up around 3 million additional people.[467] The IRS announced that it would not require that tax returns indicate that a person has health insurance, reducing the effectiveness of the individual mandate, in response to an executive order from President Donald Trump.[468] The CBO reported in March that the healthcare exchanges were expected to be stable.[418] In May the United States House of Representatives voted to repeal the ACA using the American Health Care Act of 2017.[469][470] The individual mandate was repealed starting in 2019 via the Tax Cuts and Jobs Act of 2017.[69] The CBO estimated that the repeal would cause 13 million people to lose their health insurance by 2027.[471]
Murray—Alexander Individual Market Stabilization Bill
Senator Lamar Alexander and Senator Patty Murray reached a compromise to amend the Affordable Care Act to fund cost cost-sharing reductions.[472] President Trump had stopped paying the cost sharing subsidies and the Congressional Budget Office estimated his action would cost $200 billion, cause insurance sold on the exchange to cost 20% more and cause one million people to lose insurance.[473] The plan will also provide more flexibility for state waivers, allow a new "Copper Plan" or catastrophic coverage for all, allow interstate insurance compacts, and redirect consumer fees to states for outreach.
See also
- Acronyms in healthcare
Community Living Assistance Services and Supports Act ("Class Act")- Comparison of the health care systems in Canada and the United States
- EBSA form 700
- Health care reform
- Health systems by country
- Individual shared responsibility provision
- King v. Burwell
Massachusetts health care reform (sometimes called "Romneycare")
Medicare Access and CHIP Reauthorization Act of 2015 (Reform to the American Health Care system signed into law by President Obama)- National health insurance
- Single-payer health care
- Universal health care
- Universal health coverage by country
- U.S. health care compared with 8 other countries (tabular form).
References
^ abc Wallace, Gregory (June 25, 2012). "'Obamacare': The word that defined the health care debate". CNN. Retrieved September 4, 2012..mw-parser-output cite.citationfont-style:inherit.mw-parser-output qquotes:"""""""'""'".mw-parser-output code.cs1-codecolor:inherit;background:inherit;border:inherit;padding:inherit.mw-parser-output .cs1-lock-free abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/6/65/Lock-green.svg/9px-Lock-green.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .cs1-lock-limited a,.mw-parser-output .cs1-lock-registration abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/d/d6/Lock-gray-alt-2.svg/9px-Lock-gray-alt-2.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .cs1-lock-subscription abackground:url("//upload.wikimedia.org/wikipedia/commons/thumb/a/aa/Lock-red-alt-2.svg/9px-Lock-red-alt-2.svg.png")no-repeat;background-position:right .1em center.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registrationcolor:#555.mw-parser-output .cs1-subscription span,.mw-parser-output .cs1-registration spanborder-bottom:1px dotted;cursor:help.mw-parser-output .cs1-hidden-errordisplay:none;font-size:100%.mw-parser-output .cs1-visible-errorfont-size:100%.mw-parser-output .cs1-subscription,.mw-parser-output .cs1-registration,.mw-parser-output .cs1-formatfont-size:95%.mw-parser-output .cs1-kern-left,.mw-parser-output .cs1-kern-wl-leftpadding-left:0.2em.mw-parser-output .cs1-kern-right,.mw-parser-output .cs1-kern-wl-rightpadding-right:0.2em
^ abcd Oberlander, Jonathan (June 1, 2010). "Long Time Coming: Why Health Reform Finally Passed". Health Affairs. 29 (6): 1112–1116. doi:10.1377/hlthaff.2010.0447. ISSN 0278-2715. Archived from the original on December 5, 2016.
^ abcde Blumenthal, David; Abrams, Melinda; Nuzum, Rachel (18 June 2015). "The Affordable Care Act at 5 Years". New England Journal of Medicine. 372 (25): 2451–2458. doi:10.1056/NEJMhpr1503614. ISSN 0028-4793.
^ ab Cohen, Alan B.; Colby, David C.; Wailoo, Keith A.; Zelizer, Julian E. (1 June 2015). Medicare and Medicaid at 50: America's Entitlement Programs in the Age of Affordable Care. Oxford University Press. ISBN 9780190231569.
^ ab Vicini, James; Stempel, Jonathan; Biskupic, Joan (28 June 2017). "Top court upholds healthcare law in Obama triumph". Reuters.
^ abcdef "Federal Subsidies for Health Insurance Coverage for People Under Age 65:2016 to 2026". CBO. Retrieved November 23, 2016.
^ ab "Health Insurance Coverage and the Affordable Care Act, 2010–2016". Retrieved December 7, 2016.
^ abcd "Budgetary and Economic Effects of Repealing the Affordable Care Act". Congressional Budget Office. June 18, 2015. Retrieved June 19, 2015.
^ abcd "CBO's Analysis of the Major Health Care Legislation Enacted in March 2010". Congressional Budget Office. March 30, 2011. Retrieved April 6, 2012.
^ ab CBO-The Distribution of Household Income, 2014-March 19, 2018
^ abc "Employer Health Benefits 2015". Kaiser Family Foundation. Retrieved November 19, 2016.
^ Gruber, Jonathan (2011). "The Impacts of the Affordable Care Act: How Reasonable Are the Projections?". National Tax Journal. 64 (3): 893–908. doi:10.17310/ntj.2011.3.06. Retrieved 23 July 2017.
^ ab "Analysis: U.S. Supreme Court Upholds the Affordable Care Act: Roberts Rules?". The National Law Review. von Briesen & Roper, S.C. June 29, 2012. Retrieved July 2, 2012.
^ Kirzinger, Ashley; Sugarman, Elise; Brodie, Mollyann (1 December 2016). "Kaiser Health Tracking Poll: November 2016". Kaiser Family Foundation. Retrieved 23 July 2017.
^ "Gallup: ObamaCare has majority support for first time". The Hill. Retrieved 18 November 2017.
^ Stolberg, Sheryl Gay; Pear, Robert (23 March 2010). "Obama Signs Health Care Overhaul Into Law". The New York Times.
^ Greenberg, Jon (15 January 2017). "Rand Paul goes too far on Obamacare Medicaid growth". politifact.
^ Amadeo, Kimberly. "How Much Will Obamacare Cost Me". The Balance. Retrieved November 11, 2016.
^ "The Patients' Bill of Rights: Ending annual and lifetime limits" (PDF) (Press release). FamiliesUSA. September 23, 2010. Archived from the original (PDF) on March 31, 2012. Retrieved April 9, 2012.
^ "Patient Protection and Affordable Care Act of 2009: Health Insurance Exchanges" (PDF). National Association of Insurance Commissioners. April 20, 2010. Retrieved April 9, 2012.
^ "HHS and states move to establish Affordable Insurance Exchanges, give Americans the same insurance choices as members of Congress" (Press release). HHS. July 11, 2011. Archived from the original on April 14, 2012. Retrieved April 9, 2012.
^ "Essential Health Benefits". HealthCare.gov. September 23, 2010. Retrieved February 9, 2016.
^ Cohn, Jonathan (June 12, 2013). "You Call This Insurance?". The New Republic.
^ abc Levitt, Larry; Claxton, Gary; Pollitz, Karen (October 18, 2011). "Questions About Essential Health Benefits". Kaiser Family.
^ "Essential Health Benefits". HealthCare.gov, managed by the Centers for Medicare and Medicaid Services.
"What does Marketplace health insurance cover?". HealthCare.Gov, managed by the Centers for Medicare and Medicaid Services.
^ "Preventive Services Covered Under the Affordable Care Act".
^ "Login". Retrieved February 18, 2015.
^ "Quick Take: Essential Health Benefits: What Have States Decided for Their Benchmark?". Kaiser Family. December 7, 2012.
^ PPACA, 2713,(a)(4)
^ Women's Preventive Services Guidelines HRSA, US Department of Health and Human Services
^ "Women's Preventive Services Coverage and Non-Profit Religious Organizations". Centers for Medicare and Medicaid Services. Retrieved September 8, 2013.
^ Kliff, Sarah (August 1, 2012). "Five facts about the health law's contraceptive mandate". The Washington Post. Retrieved November 29, 2012.
^ Dept. Health and Human Services (February 10, 2012). "Group Health Plans and Health Insurance Issuers Relating to Coverage of Preventive Services Under the Patient Protection and Affordable Care Act – Final Rules" (77 FR 8725). Federal Register. Retrieved February 15, 2012.Summary: These regulations finalize, without change, interim final regulations authorizing the exemption of group health plans and group health insurance coverage sponsored by certain religious employers from having to cover certain preventive health services under provisions of the Patient Protection and Affordable Care Act.
^ Park, Madison (July 19, 2011). "Birth control should be fully covered under health plans, report says". CNN. Retrieved August 27, 2012.
^ "Provisions of the Affordable Care Act, By Year". HealthCare.gov. Archived from the original on September 9, 2011. Retrieved January 9, 2012.
^ "Key Features of the Affordable Care Act By Year". HHS. June 7, 2013. Retrieved June 7, 2013.
^ ab Binckes, Jeremy; Wing, Nick (March 22, 2010). "The Top 18 Immediate Effects Of The Health Care Bill". The Huffington Post. Retrieved March 22, 2010.
^ "How do out-of-pocket maximums work?". Blue Cross Blue Shield of Michigan.
^ U.S. Department of Health and Human Services (June 28, 2010). "Patient Protection and Affordable Care Act; Requirements for Group Health Plans and Health Insurance Issuers Under the Patient Protection and Affordable Care Act Relating to Preexisting Condition Exclusions, Lifetime and Annual Limits, Rescissions, and Patient Protections; Final Rule and Proposed Rule". Federal Register. 75 (123): 37187–37241. Retrieved July 26, 2010.
^ Pool, Gentrie (October 7, 2010). "After PPACA: The Future of the Health Insurance Underwriter". Asjonline.com. Retrieved April 9, 2012.
^ "Selected Patient Protection and Affordable Care Act (PPACA) implementation dates of interest to RNs as caregivers, RNs as patients, and RNs as employees" (PDF). Nursingworld.org. Archived from the original (PDF) on May 14, 2012. Retrieved April 9, 2012.
^ "Age Band Rating (ACA)". National Association of Personal Financial Advisors.
^ Bowman, Lee (March 22, 2010). "Health reform bill will cause several near-term changes". Scripps Howard News Service. Archived from the original on December 27, 2010. Retrieved March 23, 2010.
^ "Summary of the Affordable Care Act" (PDF). Kaiser Family Foundation. April 23, 2013. Archived from the original (PDF) on October 3, 2013.
^ "Health Insurance Market Reforms: Prevention". Centers for Medicare and Medicaid Services. December 21, 2010. Retrieved September 8, 2013.
^ "Next Steps to Comply with Health Care Reform". The National Law Review. October 10, 2012. Retrieved October 10, 2012.
^ "How do I choose Marketplace insurance?". HealthCare.Gov, managed by the Centers for Medicare and Medicaid Services.
^ "Health Plan Categories". HealthCare.Gov, managed by the Centers for Medicare and Medicaid Services.
^ "Medical Loss Ratio". Centers for Medicaid and Medicare Services. Retrieved October 2, 2013.
^ "Medical Loss Ratio Requirements Under the Patient Protection and Affordable Care Act". Federal Register. December 7, 2011. p. 76573. Retrieved April 1, 2012.
^ ab "Minimum Coverage Provision ("individual mandate")". American Public Health Association (APHA). Archived from the original on July 1, 2014.
^ Galewitz, Phil (March 26, 2010). "Consumers Guide To Health Reform". Kaiser Health News.
^ Cohn, Jonathan (August 5, 2013). "Burn Your Obamacare Card, Burn Yourself". The New Republic.
^ McClanahan, Carolyn (August 4, 2013). "Reader's Questions About Obamacare – Misinformation Abounds". Forbes. Retrieved August 15, 2013.
^ ab Pippenger, Nathan (March 28, 2012). "Health Care Reform Without The Mandate?". The New Republic.
^ Cohn, Jonathan (April 9, 2010). "Common Sense". The New Republic.
Cohn, Jonathan (April 2, 2012). "What If the Mandate Goes?". The New Republic.
^ Cohn, Jonathan (July 15, 2013). "Obamacare's Individual Mandate Can't Wait". The New Republic.
Cohn, Jonathan (April 2, 2012). "What If the Mandate Goes?". The New Republic.
^ ab Cohn, Jonathan (March 21, 2012). "Reform With No Mandate? Ask New Jersey About That". The New Republic.
^ Cohn, Jonathan (June 8, 2012). "Just in Case: How Reform Might Survive Without the Mandate". The New Republic.
^ Banthin, Jessica (March 20, 2012). "Effects of Eliminating the Individual Mandate to Obtain Health Insurance". CBO.
^ ab Jonathan Gruber (economist) (February 2011). "Health Care Reform without the Individual Mandate" (PDF). Center for American Progress.
^ Eibner, Christine; Price, Carter (2012). "The Effect of the Affordable Care Act on Enrollment and Premiums, With and Without the Individual Mandate" (PDF). Rand Health.
^ Cohn, Jonathan (April 9, 2010). "Common Sense". The New Republic.
Cohn, Jonathan (April 2, 2012). "What If the Mandate Goes?". The New Republic.
Cohn, Jonathan (December 26, 2011). "Was the Mandate a Mistake?". The New Republic.
^ Cohn, Jonathan (December 26, 2011). "Was the Mandate a Mistake?". The New Republic.
^ ab "Cost Estimate for Pending Health Care Legislation" (PDF). Congressional Budget Office. March 20, 2010. Retrieved March 28, 2010.
^ ab Chaikind, Hinda; Copeland, Curtis W.; Redhead, C. Stephen; Staman, Jennifer (March 2, 2011). "PPACA: A Brief Overview of the Law, Implementation, and Legal Challenges" (PDF). Congressional Research Service. R41664. Retrieved December 22, 2013.
^ abc Trumbull, Mark (March 23, 2010). "Obama signs health care bill: Who won't be covered?". The Christian Science Monitor. Retrieved March 24, 2010.
^ Fox, Emily Jane (July 24, 2012). "6 million will lose out on Medicaid expansion". CNNMoney. Retrieved July 25, 2012.
^ abc Hatch, Orrin (December 20, 2017). "Sen. Orrin Hatch: Repealing the individual mandate tax is the beginning of the end of the ObamaCare era". Fox News. Retrieved December 21, 2017.
^ "Explaining Health Care Reform: Questions About Health Insurance Subsidies". Kaiser Family Foundation. July 1, 2012. Retrieved July 1, 2012.
^ Luhby, Tami (April 23, 2013). "Millions eligible for Obamacare subsidies, but most don't know it". CNNMoney. Retrieved June 22, 2013.
^ "Patient Protection and Affordable Care Act/Title I/Subtitle E/Part I/Subpart A".
^ Patient Protection and Affordable Care Act: Title I: Subtitle E: Part I: Subpart A: Premium Calculation
^ "Small Business Health Care Tax Credit and the SHOP Marketplace". Internal Revenue Service. October 20, 2016. Retrieved January 11, 2017.
^ "Treasury Lays the Foundation to Deliver Tax Credits" (PDF).
^ "Health Insurance Premium Credits in the PPACA" (PDF). Congressional Research Service. April 28, 2010.
^ ab "Explaining Health Care Reform". Kaiser Family Foundation.
^ "Explaining Health Care Reform" (PDF). Kaiser Family Foundation.
^ "Health Insurance Premium Credits Under PPACA" (PDF). Congressional Research Service. 2014.
^ "An Analysis of Health Insurance Premiums Under the Patient Protection and Affordable Care Act".
^ "Policies to Improve Affordability and Accountability". The White House. Archived from the original on December 30, 2012.
^ "Kaiser Family Foundation:Health Reform Subsidy Calculator – Premium Assistance for Coverage in Exchanges/Gateways".
^ "Welcome to the Marketplace". HealthCare.Gov, managed by the Centers for Medicare and Medicaid Services.
"What is the Health Insurance Marketplace?". HealthCare.Gov, managed by the Centers for Medicare and Medicaid Services.
^ "Insurance Exchanges". American Public Health Association (APHA). Archived from the original on August 1, 2013.
^ Cohn, Jonathan (April 29, 2013). "Obamacare Sticker Shock: Not Very Shocking". The New Republic.
^ ab "State Decisions For Creating Health Insurance Exchanges, as of May 28, 2013 – Notes". Kaiser Family Foundation. May 28, 2013.
^ "State Health Insurance Exchange Laws: The First Generation". The CommonWealth Fund. July 25, 2012.
^ Adams, Rebecca (July 22, 2013). "The Question of Abortion Coverage in Health Exchanges". Roll Call.
^ ab Legislative Attorneys, American Law Division (January 5, 2016), Lawsuits to Recover Payments under the Risk Corridors Program of the Affordable Care Act (PDF), Congressional Research Service, p. 6, retrieved February 11, 2017
^ ab Nicholas Bagley (November 24, 2016), "Trouble on the Exchanges – Does the United States Owe Billions to Health Insurers?", New England Journal of Medicine, 375: 2017–2019, doi:10.1056/NEJMp1612486, retrieved February 11, 2017
^ Risk Corridors and Budget Neutrality (PDF), Washington, DC: Centers for Medicare & Medicaid Services (CMS), April 11, 2014
Department of Health and Human Services
^ Yes, Marco Rubio Led The Effort To End Obamacare's Health, Forbes, December 15, 2015, retrieved February 10, 2017
^ Kessler, Glenn (December 23, 2015). "Rubio's inaccurate claim that he 'inserted' a provision restricting Obamacare 'bailout' funds". The Washington Post.
^ ab Michael Hiltzik (February 10, 2017), With billions at stake, a federal judge just nullified the GOP's most cynical attack on Obamacare, LA Times, retrieved February 10, 2017
^ Moda Health Plan, Inc. v. The United States, US Courts, February 10, 2017, p. 40, retrieved February 10, 2017
^ HHS Press Office (March 29, 2013). "HHS finalizes rule guaranteeing 100 percent funding for new Medicaid beneficiaries". Washington, D.C.: U.S. Department of Health & Human Services. Retrieved April 23, 2013.effective January 1, 2014, the federal government will pay 100 percent of defined cost of certain newly eligible adult Medicaid beneficiaries. These payments will be in effect through 2016, phasing down to a permanent 90 percent matching rate by 2020.
Centers for Medicare & Medicaid Services (April 2, 2013). "Medicaid program: Increased federal medical assistance percentage changes under the Affordable Care Act of 2010: Final rule". Federal Register. 78 (63): 19917–19947.(A) 100 percent, for calendar quarters in calendar years (CYs) 2014 through 2016; (B) 95 percent, for calendar quarters in CY 2017; (C) 94 percent, for calendar quarters in CY 2018; (D) 93 percent, for calendar quarters in CY 2019; (E) 90 percent, for calendar quarters in CY 2020 and all subsequent calendar years.
^ https://www.hhs.gov/news/press/2013pres/03/20130329a.html
^ http://www.cbpp.org/cms/?fa=view&id=3801
^ "Medicaid Expansion". Is Medicaid eligibility expanding to 133 or 138 percent FPL, and what is MAGI?: American Public Health Association (APHA). Archived from the original on February 22, 2014. Retrieved July 24, 2013.
^ ab "Affordable Care Act Update: Implementing Medicare Cost Savings" (PDF). Centers for Medicare and Medicaid Services. August 2, 2010. Archived from the original (PDF) on April 18, 2013. Retrieved October 7, 2013.
^ "Higher Spending Relative to Medicare Fee-for-Service May Not Ensure Lower Out-of-Pocket Costs for Beneficiaries". Government Accountability Office. February 8, 2008. Retrieved October 7, 2013.
^ "PPACA, section 9015 as modified by section 10906" (PDF).
^ "HCERA section 1402" (PDF).
^ Nowak, Sarah; Eibner, Christine (December 18, 2015). "Rethinking the Affordable Care Act's "Cadillac Tax": A More Equitable Way to Encourage "Chevy" Consumption". Commonwealth Fund.
^ "Briefing Book". Tax Policy Center.
^ "Where are States Today? Medicaid and CHIP Eligibility Levels for Children and Non-Disabled Adults". Kaiser Family Foundation. March 28, 2013.
^ H.R. 3590 Enrolled, section 1001 (adding section 2714 to the Public Health Service Act): "A group health plan and a health insurance issuer offering group or individual health insurance coverage that provides dependent coverage of children shall continue to make such coverage available for an adult child (who is not married) until the child turns 26 years of age."
^ "Young Adults and the Affordable Care Act" (PDF). Archived from the original (PDF) on November 11, 2016.
^ "Explaining Health Care Reform: What is Employer "Pay-or-Play" Requirement?". Kaiser Family Foundation. May 1, 2009. Retrieved January 9, 2012.
^ McNamara, Kristen (March 25, 2010). "What Health Overhaul Means for Small Businesses". The Wall Street Journal.
^ Cohn, Jonathan (May 21, 2013). "Weaseling Out of Obamacare". The New Republic.
^ "Health Coverage & Uninsured". Kaiser Family Foundation. June 20, 2013.
"Health Insurance Coverage of the Total Population". Kaiser Family Foundation. June 20, 2013.
^ "Pg 14 of 'Kaiser Health Tracking Poll: June 2013'" (PDF). Kaiser Family Foundation. June 2013.
^ Chait, Jonathan (May 29, 2013). "Yuval Levin Dissembles Madly". New York.
^ "Access". Medscape. Retrieved January 9, 2012.
(registration required)
^ "Key Healthcare Reform Initiatives: Medicare Bundled Payment Pilots". Huron Consulting Group. November 19, 2010. Retrieved January 9, 2012.
^ "More savings in the drug coverage gap coming through 2020". Centers for Medicare & Medicaid Services. Retrieved September 27, 2013.
^ abc "Accountable Care Organizations, Explained". Kaiser Health News. September 14, 2015. Retrieved August 18, 2016.
^ "What the Affordable Care Act means for prescription coverage". Washington Post. Retrieved August 7, 2016.
^ Claffey, Jason (August 14, 2010). "Medicare 'Doughnut Hole' Checks in the Mail". Foster's Daily Democrat. Retrieved December 26, 2012.
^ "Closing the Coverage Gap – Medicare Prescription Drugs Are Becoming More Affordable" (PDF). CMS. January 2015. Archived from the original (PDF) on May 23, 2013.
^ ab "Public Law 111 – 148, section 1332". Government Printing Office. Retrieved June 29, 2012.
^ "Preparing for Innovation: Proposed Process for States to Adopt Innovative Strategies to Meet the Goals of the Affordable Care Act". U.S. Department of Health & Human Services. November 16, 2011. Retrieved April 1, 2012.
^ Goldstein, Amy; Balz, Dan (March 1, 2011). "Obama offers states more flexibility in health-care law". The Washington Post.
^ "Gov. Shumlin issued the following statement on health care rules". Governor.vermont.gov. March 14, 2011. Archived from the original on May 16, 2013. Retrieved April 1, 2012.
^ Estes, Adam Clark (May 26, 2011). "Vermont Becomes First State to Enact Single-Payer Health Care". The Atlantic. Retrieved April 1, 2012.
^ Wing, Nicholas (May 26, 2011). "Vermont Single-Payer Health Care Law Signed By Governor". The Huffington Post.
^ "Costs derail Vermont's single-payer health plan". The Boston Globe.
^ Span, Paula (March 29, 2010). "Options Expand for Affordable Long-Term Care". The New York Times. Retrieved March 29, 2010.
^ PriceWaterHouseCoopers. "The CLASS Act." HRS Insight: Human Resource Services. 2010: 1–6. Web.
^ Carney, Timothy (February 28, 2011) So, yeah, the health-care bill was really an awful piece of legislation that sent the revolving door spinning faster[permanent dead link], Washington Examiner
^ "Consumer Operated and Oriented Plans (CO-OPs)".
^ Affordable Care Act's calorie count rules go into effect
^ abcd Roy, Avik (February 7, 2012). "The Tortuous History of Conservatives and the Individual Mandate". Forbes Magazine.
^ Butler, Stuart M. (1989). (PDF). The Heritage Foundation http://healthcarereform.procon.org/sourcefiles/1989_assuring_affordable_health_care_for_all_americans.pdf. Missing or empty|title=(help)
^ Cohn, Jonathan (April 9, 2010). "Common Sense". The New Republic.
^ abc Cooper, Michael (February 14, 2012). "Conservatives Sowed Idea of Health Care Mandate, Only to Spurn It Later". The New York Times. Retrieved July 2, 2012.
^ abc Klein, Ezra (June 25, 2012). "Unpopular Mandate". The New Yorker. Retrieved June 19, 2012.
^ Cohn, Bob; Clift, Eleanor (September 18, 1994). "The Lost Chance". Newsweek. Retrieved July 2, 2012.
^ Fouhy, Beth (October 5, 2007). "Hillary Claims Credit for Child Program". Associated Press for NewsMax. Archived from the original on January 23, 2008.
^ ab "Chart: Comparing Health Reform Bills: Democrats and Republicans 2009, Republicans 1993". Kaiser Health News. February 23, 2010. Retrieved July 29, 2012.
"Summary Of A 1993 Republican Health Reform Plan". Kaiser Health News. February 23, 2010. Retrieved July 29, 2012.
^ "In 1993, Republicans Proposed A Mandate First". NPR. March 31, 2012.
^ "History of the Individual Health Insurance Mandate, 1989–2010 Republican Origins of Democratic Health Care Provision". ProCon.org. February 9, 2012.
^ ab "Facebook post says Republicans embraced individual mandate in 1993". PolitiFact. April 19, 2012.
^ "AG Suthers couldn't be more wrong in his decision to file lawsuit". Colorado Statesman. Retrieved July 29, 2012.
^ "G.O.P. and Health Mandate". The New York Times. February 26, 2012.
^ "Romneycare's 98% Success Rate Defies Gripes on Obama Law". Bloomberg. March 26, 2012.
^ Ball, Molly (May 31, 2012). "Was Mitt Romney a Good Governor?". The Atlantic. Retrieved October 28, 2013.
^ ab Lizza, Ryan (June 6, 2011). "Romney's dilemma". The New Yorker. Retrieved June 19, 2012.
^ "Bill Summary & Status – S.334". Library of Congress THOMAS. Retrieved September 24, 2013.
^ Kuttner, Robert (June 28, 2011). "RomneyCare vs. ObamaCare". The Boston Globe. Retrieved September 23, 2013.
^ Cline, Andrew. "How Obama Broke His Promise on Individual Mandates". The Atlantic. Retrieved September 26, 2013.
^ "CNN Democratic presidential debate". CNN. January 21, 2008. Retrieved September 26, 2013.
^ "The First Presidential Debate". The New York Times. September 26, 2008.
^ Rustgi, Sheila; Collins, Sara R.; Davis, Karen; Nicholson, Jennifer L. "The 2008 Presidential Candidates' Health Reform Proposals: Choices for America".
^ "Remarks of President Barack Obama – Address to Joint Session of Congress". The White House. February 24, 2009. Archived from the original on March 8, 2010. Retrieved March 24, 2010.
^ abcde "Timeline: Milestones in Obama's quest for healthcare reform". Reuters. March 22, 2010. Retrieved March 22, 2010.
^ Kruger, Mike (October 29, 2009). "Affordable Health Care for America Act". United States House Committee on Education and Labor. Archived from the original on January 6, 2010. Retrieved March 24, 2010.
^ "Health Care Reform from Conception to Final Passage". Retrieved November 23, 2010.
^ "Senate Finance Committee Hearings for the 111th Congress recorded by C-SPAN". C-SPAN.
[permanent dead link]
^ "Senate Finance Committee hearings for 111th Congress". Finance.Senate.Gov. Archived from the original on January 11, 2013. Retrieved April 1, 2012.
^ "Jonathan Gruber (economist)". MIT Department of Economics. Retrieved September 2, 2013.
"Jonathan Gruber: short biography". MIT Department of Economics. Archived from the original on September 28, 2013. Retrieved September 2, 2013.
^ ab Cohn, Jonathan (May 21, 2010). "How They Did It". The New Republic.
^ Cohn, Jonathan (September 4, 2009). "Party Is Such Sweet Sorrow". The New Republic.
^ Chait, Jonathan (April 22, 2010). "Obama's Moderate Health Care Plan". The New Republic.
Chait, Jonathan (December 19, 2009). "The Republican Health Care Blunder". The New Republic.
^ Chait, Jonathan (December 19, 2009). "The Republican Health Care Blunder". The New Republic.
^ Hulse, Carl; Nagourney, Adam (March 16, 2010). "Senate G.O.P. Leader Finds Weapon in Unity". The New York Times.
^ Eaton, Joe; Pell, M. B.; Mehta, Aaron (March 26, 2010). "Lobbying Giants Cash In On Health Overhaul". NPR. Retrieved April 9, 2012.
^ Cohn, Jonathan (August 25, 2009). "Drug Deal". The New Republic.
^ Grim, Ryan (August 13, 2009). "Internal Memo Confirms Big Giveaways In White House Deal With Big Pharma". The Huffington Post.
^ "Visualizing The Health Care Lobbyist Complex". Sunlight Foundation. July 22, 2009. Retrieved April 1, 2012.
^ Horwitz, Sari; Pershing, Ben (April 9, 2010). "Anger over health-care reform spurs rise in threats against Congress members". The Washington Post. Retrieved April 9, 2010.
^ Kellman, Laurie; Abrams, Jim (March 26, 2010). "Threats against lawmakers spread after health vote". Associated Press.
^ "Remarks by the President to a Joint Session of Congress on Health Care". The White House. September 10, 2009. Archived from the original on March 8, 2010. Retrieved March 24, 2010.
^ Kennedy, Edward M. (May 12, 2009). "Text of letter to the President from Senator Edward M. Kennedy". White House Press Secretary. Archived from the original on September 10, 2009. Retrieved September 10, 2009.
^ U.S. Const. art. I, § 7, cl. 1.
^ "Summary: H.R.3590 — 111th Congress (2009–2010)". Library of Congress. July 30, 2017.
^ S.Amdt. 2786
^ Cohn, Jonathan (September 7, 2009). "Why Reform Survived August". The New Republic.
^ Hacker, Jacob S. (December 20, 2009). "Why I Still Believe in This Bill". The New Republic.
^ ab Cohn, Jonathan (March 12, 2010). "The Public Option, Still Dead". The New Republic.
^ Cohn, Jonathan (December 15, 2009). "What Public Option Supporters Won". The New Republic.
^ Cohn, Jonathan (December 17, 2009). "Ben Nelson, Still a Big Problem (Updated)". The New Republic.
^ Cohn, Jonathan (December 19, 2009). "Nelson Says Yes; That Makes 60". The New Republic.
^ "'Cornhusker' Out, More Deals In: Health Care Bill Gives Special Treatment". Fox News. March 19, 2010. Retrieved April 26, 2010.
^ "Roll Call vote No. 395 – On the Cloture Motion (Motion to Invoke Cloture on H.R. 3590)". U.S. Senate. Retrieved July 20, 2017.
^ "Roll Call vote No. 396 – On Passage of the Bill (H.R. 3590 as Amended)". U.S. Senate. Retrieved January 9, 2012.
^ "AARP, AMA Announce Support For Health Care Bill: Largest Doctors And Retiree Groups Backing Legislation". The Huffington Post, March 19, 2010.
^ Applewhite, J. Scott. "Senator-elect Scott Brown welcomed as Republican hero after upset victory in Massachusetts". McClatchy-Tribune News Service. Associated Press. Retrieved April 19, 2012.
^ "Public Statements – Project Vote Smart" (Press release). Votesmart.org. January 13, 2010. Retrieved April 9, 2012.
^ Silver, Nate (January 21, 2010). "Will the Base Abandon Hope?". FiveThirtyEight.
^ ab Cohn, Jonathan (January 17, 2010). "How to Pass the Bill--Whatever Happens Tuesday". The New Republic.
^ abc Stolberg, Sheryl; Zeleny, Jeff; Hulse, Carl (March 20, 2010). "Health Vote Caps a Journey Back From the Brink". The New York Times. Retrieved March 23, 2010.
^ ab Brown, Carrie; Thrush, Glenn (March 20, 2010). "Pelosi steeled W.H. for health push". Politico. Retrieved March 23, 2010.
^ "White House Unveils Revamped Reform Plan, GOP And Industry React". Kaiser Health News. February 22, 2010. Retrieved June 29, 2012.
^ ab Chait, Jonathan (February 20, 2010). "A Brief Reconciliation Primer". The New Republic.
^ ab Silver, Nate (December 26, 2009). "For Pelosi, Many Paths to 218". FiveThirtyEight.
^ Silver, Nate (January 21, 2010). "1. Reconciliation! 2. ??? 3. Profit!". FiveThirtyEight.
^ Cohn, Jonathan (September 21, 2009). "Reconciliation: Why Most Dems Don't Want to Go There". The New Republic.
^ Executive Order 13535 of March 24, 2010 — Ensuring Enforcement and Implementation of Abortion Restrictions in the Patient Protection and Affordable Care Act, Vol. 75, No. 59 75 FR 15599, March 29, 2010.
^ Chait, Jonathan (March 21, 2010). "Stupak Makes A Deal, Reform To Pass". The New Republic.
^ "Roll Call vote No. 165: On Motion to Concur in Senate Amendments (Patient Protection and Affordable Care Act)". Office of the Clerk: House of Representatives. March 21, 2010. Retrieved April 9, 2012.
^ Aro, Margaret; Mooney, Mark (March 22, 2010). "Pelosi Defends Health Care Fight Tactics". ABC News. Retrieved March 23, 2010.
^ Stolberg, Sheryl; Pear, Robert (March 23, 2010). "Obama Signs Health Care Overhaul Bill, With a Flourish". The New York Times. Retrieved March 24, 2010.
^ Benen, Steve (February 2, 2016). "On Groundhog Day, Republicans vote to repeal Obamacare". MSNBC.
^ "National Health Interview Survey, January to June 2016" (PDF). CDC.gov. Retrieved November 23, 2016.
^ Barry-Jester, Anna Maria; Ben, Casselman (September 22, 2016). "Obamacare Has Increased Insurance Coverage Everywhere". FiveThirtyEight. Retrieved October 12, 2016.
^ Garrett, Bowen (December 2016). "Who Gained Health Insurance Coverage Under the ACA, and Where Do They Live?" (PDF). Urban Institute. p. 2. Retrieved 22 April 2017.
^ ab "Health Reform Monitoring Survey". Retrieved December 5, 2016.
^ ab "Current Status of State Medicaid Expansion Decisions". Retrieved December 5, 2016.
^ "Rates Up 22 Percent For Obamacare Plans, But Subsidies Rise, Too". Retrieved November 19, 2016.
^ ab "Average Annual Workplace Family Health Premiums Rise Modest 3%". Kaiser Family Foundation. Retrieved November 23, 2016.
^ "The Economic Record of the Obama Administration: Progress Reducing Inequality" (PDF). Whitehouse.gov. Archived from the original (PDF) on November 26, 2016. Retrieved December 6, 2016.
^ https://www.fool.com/taxes/2018/01/07/what-the-individual-mandate-repeal-means-for-the-a.aspx
^ https://www.fool.com/taxes/2018/01/07/what-the-individual-mandate-repeal-means-for-the-a.aspx
^ https://www.taxpolicycenter.org/briefing-book/what-tax-changes-did-affordable-care-act-make
^ https://money.cnn.com/2018/03/03/news/economy/obamacare-tax-penalty/index.html
^ Nussbaum, Alex (March 4, 2015). "Health Insurance Exchanges". Bloomberg View. Retrieved August 12, 2016.
^ "Status of State Action on the Medicaid Expansion Decision, as of September 1, 2015". Kaiser Family Foundation. June 22, 2015.
^ ab Robert Pear (May 24, 2013). "States' Policies on Health Care Exclude Some of the Poorest". The New York Times. Retrieved May 25, 2013.In most cases, [Sandy Praeger, Insurance Commissioner of Kansas], said adults with incomes from 32 percent to 100 percent of the poverty level ($6,250 to $19,530 for a family of three) "will have no assistance".
^ ab "Cost of Obamacare Medicaid Expansion 49% Higher Than Previously Estimated". August 12, 2016. Retrieved August 13, 2016.
^ "The Impact of the Coverage Gap for Adultsin States not Expanding Medicaid". October 26, 2015.
^ Kliff, Sarah (July 5, 2012). "What Happens if a State Opts Out of Medicaid, in One Chart". The Washington Post. Retrieved July 15, 2012.
^ "Health Reform and MedicaidExpansion". HealthCare Reform Magazine. July 13, 2010. Retrieved January 9, 2012.
^ "Analyzing the Impact of State Medicaid Expansion Decisions". Kaiser Family Foundation. July 17, 2013.
^ "Enrollment Policy Provisions in the Patient Protection and Affordable Care Act" (PDF). Families USA. Retrieved April 1, 2012.
^ Cohn, Jonathan (July 19, 2013). "We Don't Know Everything About Obamacare. But We Know Who's Trying to Sabotage It". The New Republic.
^ ab Tami Luhby (July 1, 2013). "States forgo billions by opting out of Medicaid expansion". CNN.
^ "Is Medicaid Expansion Good for the States?". U.S. News & World Report. n.d.
^ Evan Soltas (June 4, 2013). "Wonkbook: The terrible deal for states rejecting Medicaid". The Washington Post.
^ Rutkin, Aviva. "Obamacare has already improved health of low-income Americans". Retrieved August 15, 2016.
^ "Medicaid expansion under ACA linked with better health care, improved health for low-income adults | News | Harvard T.H. Chan School of Public Health". www.hsph.harvard.edu. Retrieved August 30, 2016.
^ Sanger-katz, Margot (August 25, 2016). "How Expanding Medicaid Can Lower Insurance Premiums for All". The New York Times. ISSN 0362-4331. Retrieved September 4, 2016.
^ "NationalHealthAccountsProjected". February 15, 2017.
^ Mali, Meghashyam (August 11, 2016). "Next president faces possible ObamaCare meltdown". Retrieved August 15, 2016.
^ "2017 Premium Changes and Insurer Participation in the Affordable Care Act's Health Insurance Marketplaces". Kaiser Family Foundation. Retrieved November 23, 2016.
^ "New Analysis of Health Insurance Premium Trends in the Individual Market Finds Average Yearly Increases of 10 Percent or More Prior to the Affordable Care Act". Commonwealth Fund. June 5, 2014.
^ Lowrey, Annie (May 7, 2013). "Slowdown in Rise of Healthcare Costs May Persist". The New York Times. Retrieved June 10, 2013.
^ Chait, Jonathan (May 10, 2013). "The Facts Are In and Paul Ryan Is Wrong". New York.
^ Chait, Jonathan (September 26, 2013). "Someone Tell Ted Cruz the Obamacare War Is Over". New York.
^ Wayne, Alex (June 18, 2013). "Health Cost Growth Slows Further Even as Economy Rebounds". Bloomberg L.P.
^ "Assessing the Effects of the Economy on the Recent Slowdown in Health Spending". Kaiser Family Foundation. April 22, 2013.
^ Krawzak, Paul (June 14, 2013). "In Spending Debate, Baby Boomer Issue Remains a Headache for Legislators". Roll Call.
^ Obama, B, JD. United States Health Care Reform – Progress to Date and Next Steps. JAMA. Published online July 11, 2016. doi:10.1001/jama.2016.9797
^ Johnson, Carolyn Y. (September 14, 2016). "How companies are quietly changing your health plan to make you pay more". Washington Post. Retrieved September 14, 2016.
^ "Survey of Non-Group Health Insurance Enrollees, Wave 3". kff.org. Kaiser Family Foundation. May 20, 2016. Retrieved September 14, 2016.
^ abc The FRED Blog-There's Death and then there's Death-Nov 2, 2017
^ ab "Obama's claim the Affordable Care Act was a 'major reason' in preventing 50,000 patient deaths". Washington Post. Retrieved November 10, 2016.
^ "Repealing the Affordable Care Act will kill more than 43,000 people annually". Washington Post. Retrieved 2017-01-23.
^ ab Kaiser Family Foundation-The Coverage Gap: Uninsured Poor Adults in States that Do Not Expand Medicaid-November 1, 2017
^ Elmendorf, Douglas W. (March 30, 2011). "CBO's Analysis of the Major Health Care Legislation Enacted in March 2010" (PDF). Congressional Budget Office. Retrieved July 15, 2012.
^ Elmendorf, Douglas W. (June 21, 2011). "CBO's 2011 Long-Term Budget Outlook" (PDF). Congressional Budget Office. p. 44.Through those changes and numerous others, the 2010 legislation significantly decreased Medicare outlays relative to what they would have been under prior law.
^ "Another Comment on CBO's Estimates for the Insurance Coverage Provisions of the Affordable Care Act". Congressional Budget Office. March 16, 2012. Retrieved April 6, 2012.
^ "H.R. 4872, Reconciliation Act of 2010" (PDF). Congressional Budget Office. March 18, 2010. Retrieved March 22, 2010.
^ Dennis, Steven (March 18, 2010). "CBO: Health Care Overhaul Would Cost $940 Billion". Roll Call. Retrieved March 22, 2010.
^ Klein, Ezra (March 22, 2010). "What does the health-care bill do in its first year?". The Washington Post.
^ ab "Correction Regarding the Longer-Term Effects of the Manager's Amendment to the Patient Protection and Affordable Care Act" (PDF). Congressional Budget Office. December 19, 2009. Retrieved March 22, 2010.
^ Judith Solomon; Paul N. Van de Water (April 18, 2012). "Letter: Improving the Strength and Solvency of Medicare". The Center on Budget and Policy Priorities.
^ Pecquet, Julian (March 13, 2012). "CBO: Obama's health law to cost less, cover fewer people than first thought". The Hill. Retrieved June 29, 2012.
^ "CBO's Estimates for the Insurance Coverage Provisions of the Affordable Care Act Updated for the Recent Supreme Court Decision". Congressional Budget Office. July 24, 2012. Retrieved August 6, 2012.
^ Sahadi, Jeanne (March 13, 2012). "Health reform coverage cost falls slightly". CNN. Retrieved June 29, 2012.
^ "Where does health care reform stand?". CNN. March 18, 2010. Retrieved May 12, 2010.
^ Farley, Robert (March 18, 2010). "Pelosi: CBO says health reform bill would cut deficits by $1.2 trillion in second decade". PolitiFact.com. Retrieved April 7, 2010.
^ "Sen. Tom Coburn: Obamacare PR campaign anchored in spin, not reality". The Washington Examiner. July 8, 2006. Archived from the original on July 17, 2012. Retrieved April 1, 2012.
^ James Capretta. "Obamacare's Cooked Books and the 'Doc Fix'". National Review.
^ Hogberg, David (November 22, 2010). "GOP Might Target ObamaCare As Part Of A Medicare 'Doc Fix'". Investor's Business Daily. Retrieved April 1, 2012.
^ "Responses to Questions About CBO's Preliminary Estimate of the Direct Spending and Revenue Effects of H.R. 4872, the Reconciliation Act of 2010" (PDF). Congressional Budget Office. March 19, 2010. Retrieved April 1, 2012.
^ Chait, Jonathan (March 24, 2010). "The Doc Fix Myth And The Right's Misinformation Feedback Loop". The New Republic.
^ Van de Water, Peter. "Debunking False Claims About Health Reform, Jobs, and the Deficit". Center for Budget and Policy Priorities.
^ Uwe Reinhardt (March 24, 2010). "Wrapping Your Head Around the Health Bill". The New York Times. Retrieved October 9, 2010.
^ Holtz-Eakin, Douglas (March 21, 2010). "The Real Arithmetic of Health Care Reform". The New York Times.
^ ab Cohn, Jonathan (January 21, 2011). "The GOP's Trick Play". The New Republic.
^ Scheiber, Noam (September 17, 2009). "Is the CBO Biased Against Health Care Reform?". The New Republic.
^ "Electronic Medical Records (Health Information Technology)".
^ James, Frank (March 19, 2010). "Health Overhaul Another Promise U.S. Can't Afford: Expert". NPR. Retrieved April 7, 2010.
^ "Congress Has Good Record of Implementing Medicare Savings". CBPP. Retrieved March 28, 2010.
^ "Can Congress cut Medicare costs?". The Washington Post. Retrieved March 28, 2010.
^ "The Affordable Care Act and Employers". Retrieved August 11, 2016.
^ "Is the Affordable Care Act a Hidden Jobs Killer?". Center for Economic and Policy Research. CEPR. Retrieved August 26, 2015.
^ Cohn, Jonathan (February 11, 2011). "Sorry, The CBO Did Not Say Health Reform Kills 800,000 Jobs". The New Republic.
^ Cohn, Jonathan (June 13, 2012). "Obamacare, Good for the Economy". The New Republic.
^ ab Government Printing Office. "Title 26 – Internal Revenue Code" (PDF).
^ ab Chait, Jonathan (July 3, 2013). "Obama Employer Mandate Delay Train Wreck! Or Not". New York.
^ abcd Sarah Kliff (May 6, 2013). "Will Obamacare lead to millions more part-time workers? Companies are still deciding". The Washington Post.
^ ab Ungar, Rick. "The Real Numbers On 'The Obamacare Effect' Are In-Now Let The Crow Eating Begin". Forbes. Retrieved November 11, 2014.
^ "Employment Situation Summary". Bureau of Labor Statistics. Retrieved November 11, 2014.
^ Conover, Chris. "Who Can Deny It? Obamacare Is Accelerating U.S. Towards A Part-Time Nation". Forbes. Retrieved November 11, 2014.
^ Moriya, A. S.; Selden, T. M.; Simon, K. I. (January 5, 2016). "Little Change Seen In Part-Time Employment As A Result Of The Affordable Care Act". Health Affairs. 35 (1): 119–123. doi:10.1377/hlthaff.2015.0949.
^ Bill Sizemore (February 8, 2013). "Va. workers' part-time hours capped due to health law". The Virginian-Pilot.
Annie-Rose Strasser (February 11, 2013). "Virginia Cuts State Employees' Hours To Avoid Providing Obamacare Coverage". ThinkProgress.
^ Ned Resnikoff (January 14, 2013). "Colleges roll back faculty hours in response to Obamacare". MSNBC.
Sy Mukherjee (January 14, 2013). "Four Public Colleges Will Cut Adjunct Faculty Hours To Avoid Providing Health Coverage Under Obamacare". ThinkProgress.
^ ab "As Health Law Changes Loom, A Shift To Part-Time Workers". NPR. April 29, 2013.
^ Jared Bernstein (September 4, 2013). "Stop Blaming Obamacare for Part-Time Workers". Teagan Goddard's Wonkwire. Archived from the original on July 15, 2014.
^ Matthew Yglesias (July 15, 2013). "Obamacare's Not To Blame For Increasing Part-time Work". Slate.
^ Timothy Jost (July 2, 2013). "Implementing Health Reform: A One-Year Employer Mandate Delay". Health Affairs.
^ abc Cohn, Jonathan (July 2, 2013). "Some Bad News About Obamacare That Isn't Bogus". The New Republic.
^ "Am I eligible for coverage in the Marketplace?". HealthCare.Gov, managed by the Centers for Medicare and Medicaid Services.
^ ab Robert Greenstein; Judith Solomon (July 3, 2013). "Finance Committee Makes Flawed Employer Requirement in Health Reform Bill Still More Problematic". Center on Budget and Policy Priorities.
^ abcd Ezra Klein (July 2, 2013). "Will Obamacare lead to millions more part-time workers? Companies are still deciding". The Washington Post.
^ Matthew Yglesias (July 3, 2013). "Delaying Employer Responsibility Fines Is a Good Idea—the Real Problem Comes Later". Slate.
^ Chait, Jonathan (July 3, 2013). "Obamacare Haters Struggling to Understand What 'Nonessential' Means". New York.
Chait, Jonathan (July 3, 2013). "Obamacare Still Not Collapsing". New York.
^ Cohn, Jonathan (July 15, 2013). "Obamacare's Individual Mandate Can't Wait". The New Republic.
^ "Union Letter: Obamacare Will 'Destroy The Very Health and Wellbeing' of Workers", The Wall Street Journal, July 12, 2013.
^ Torres, Carlos (January 27, 2014). "Economists See Little Effect on Hiring From U.S. Health-Care Law". www.businessweek.com. Bloomberg L.P. Retrieved January 27, 2014.
^ O'Donnell, Jayne; Ungar, Laura; Hoyer, Meghan (November 12, 2014). "Rural hospitals in critical condition". USA Today. Retrieved January 28, 2015.
Hamada, Omar L. (November 18, 2014). "Obamacare has detrimental effect on rural hospitals". The Tennessean. Retrieved January 28, 2015.
^ Howell, Tom Jr. (May 4, 2015). "ER visits up under Obamacare despite promises, doctors' poll finds". The Washington Times. Retrieved May 6, 2015.
^ "Obama and Democrats' Health Care Plan". RealClearPolitics. October 13, 2013. Retrieved March 26, 2014.
^ Swanson, Emily (July 30, 2009). "Health Care Plan: Favor/Oppose". Pollster.com.
^ "As Health Care Law Proceeds, Opposition and Uncertainty Persist" (PDF). Pew Research Center. September 16, 2013.
^ Page, Susan (March 24, 2010). "Poll: Health care plan gains favor". USA Today. Retrieved March 24, 2010.
^ ab Zengerle, Patricia (June 24, 2012). "Reuters-Most Americans Oppose Health Law But Like the Provisions". Reuters. Retrieved June 28, 2012.
^ Ezra Klein (June 26, 2012). "Republicans hate 'Obamacare', but like most of what it does". The Washington Post. Retrieved June 28, 2012.
^ Greg Sargent (June 25, 2012). "Republicans Support Obama's Health Reforms – As Long As His Name Isn't On Them". The Washington Post. Retrieved June 28, 2012.
^ "CNN Opinion Research Poll" (PDF). CNN. March 22, 2010.
^ Rasmussen, Scott; Schoen, Doug (March 9, 2010). "Why Obama Can't Move the Health-Care Numbers". The Wall Street Journal.
^ Chait, Jonathan (June 13, 2013). "Obamacare, Public Opinion, and Conservative Self-Delusion". New York Magazine.
^ Jackson, David. "Poll: Most oppose blocking Obama health care law". USA Today. Retrieved July 8, 2012.
^ "RAND Health Reform Opinion Study". RAND Health. May 1, 2014. Retrieved May 10, 2014.
^ "AP-GfK Poll: Obama's health care fails to gain support". Associated Press. March 28, 2014. Retrieved March 30, 2014.
^ "The ObamaCare 8%". The Wall Street Journal. April 30, 2014. Retrieved May 1, 2014.
^ Alan Colmes, "Poll: Voters No Longer Want To Repeal Obamacare", Liberaland, December 1, 2014.
^ "Poll: Obamacare and the Supreme Court". CBS News. Retrieved June 23, 2015.
^ "After the Election, the Public Remains Sharply Divided on Future of the Affordable Care Act". Kaiser Family Foundation. December 3, 2016.
^ "Obamacare More Popular Than Ever, Now That It May Be Repealed". NYT. February 1, 2017.
^ abc Dropp, Kyle; Nyhan, Brendan (2017-02-07). "One-Third Don't Know Obamacare and Affordable Care Act Are the Same". The New York Times. ISSN 0362-4331. Retrieved 2017-02-08.
^ Lerman, Amy E.; McCabe, Katherine T. (2017-01-24). "Personal Experience and Public Opinion: A Theory and Test of Conditional Policy Feedback". The Journal of Politics: 000–000. doi:10.1086/689286. ISSN 0022-3816.
^ Amanda Cox; Alicia Desantis; Jeremy White (March 25, 2012). "Fighting to Control the Meaning of 'Obamacare'". The New York Times. Retrieved June 29, 2012.
^ ab Baker, Peter (August 3, 2012). "Democrats Embrace Once Pejorative 'Obamacare' Tag". The New York Times. Retrieved August 6, 2012.
^ Nelson, Steven (June 8, 2011). "Democratic Rep. John Conyers wants to reclaim 'ObamaCare', make it a compliment". The Daily Caller. Retrieved April 1, 2012.
^ Madison, Lucy (August 15, 2011). "On bus tour, Obama embraces 'Obamacare', says 'I do care'". CBS News. Retrieved April 28, 2012.
^ Strauss, Daniel (March 23, 2012). "Obama camp's pitch to supporters: 'Hell yeah, I'm for Obamacare'". The Hill. Retrieved March 27, 2012.
^ Prince, Richard (October 2, 2013). "AP, NPR Curb Use of "Obamacare" Term". Robert C. Maynard Institute for Journalism Education. Archived from the original on October 5, 2013. Retrieved October 5, 2013.
^ Gold, Hadas (October 4, 2013). "AP, NPR to cut back on 'Obamacare'". Politico. Retrieved October 19, 2013.
^ ab "Sarah Palin falsely claims Barack Obama runs a "death panel"". PolitiFact. August 10, 2009.
^ "Seniors Beware". Snopes. August 23, 2012.
^ Beutler, Brian (August 13, 2013). "A new kind of birther and death panel insanity explodes". Salon. Retrieved December 3, 2013.
^ Ebeler, Jack; Neuman, Tricia; Cubanski, Juliette (April 13, 2011). "The Independent Payment Advisory Board: A New Approach to Controlling Medicare Spending". Kaiser Family Foundation. p. 3. Retrieved November 27, 2013.
^ Cohn, Jonathan (April 20, 2011). "Here We Go Again, With the Death Panels". The New Republic.
^ Cohn, Jonathan (August 13, 2009). "Mandatory Death Counseling – exposed!". The New Republic.
^ Parsons, Christi; Zajac, Andrew (August 14, 2009). "Senate committee scraps healthcare provision that gave rise to 'death panel' claims; Though the claims are widely discredited, the Senate Finance Committee is withdrawing from its bill the inclusion of advance-care planning consultations, calling them too confusing". Los Angeles Times.
^ Nyhan, Brendan (2010). "Why the "Death Panel" Myth Wouldn't Die: Misinformation in the Health Care Reform Debate" (PDF). The Forum. Berkeley Electronic Press. 8 (1). doi:10.2202/1540-8884.1354.
^ Viebeck, Elise (September 26, 2012). "Poll: Four in 10 believe in Obama healthcare law 'death panels'". The Hill.
^ Drobnic Holan, Angie (December 19, 2009). "PolitiFact's Lie of the Year: 'Death panels'". PolitiFact. Retrieved November 19, 2010.
^ Henig, Jess; Robertson, Lori (July 29, 2010). "False Euthanasia Claims". FactCheck.org.
^ Lori Robertson (December 24, 2009). "Whoppers of 2009—We review the choicest falsehoods from a year that kept us busy". FactCheck.org. Retrieved April 28, 2011.
^ "'Tweet' 2009 Word of the Year, 'Google' Word of the Decade, as voted by American Dialect Society" (PDF). American Dialect Society. January 8, 2010. Retrieved October 8, 2010.
^ "Euthanasia Counseling". Snopes. August 13, 2009.
^ Public Law 111 – 148, section 1312: "... the only health plans that the Federal Government may make available to Members of Congress and congressional staff with respect to their service as a Member of Congress or congressional staff shall be health plans that are (I) created under this Act (or an amendment made by this Act); or (II) offered through an Exchange established under this Act (or an amendment made by this Act)."
^ Chait, Jonathan (August 6, 2013). "Congress Exempts Itself From Obamacare! Or Something!". New York.
^ Cohn, Jonathan (August 13, 2013). "The Latest Obamacare Lie That Just Won't Die". The New Republic.
^ Bowers, Becky (August 14, 2013). "Sen. Ted Cruz says Obama 'just granted all of Congress an exception' to Obamacare". PolitiFact. Retrieved August 19, 2013.
^ Robertson, Lori (January 20, 2010). "Congress Exempt from Health Bill?". FactCheck.org.
^ Viebeck, Elise (February 27, 2013). "Poll: Four in 10 think illegals are covered by Obama healthcare law". The Hill. Retrieved December 7, 2013.
^ Farley, Robert (January 21, 2010). "The Democrats' health care bills would provide 'free health care for illegal immigrants'". PolitiFact. Retrieved August 19, 2013.
^ "The Once and Future Obamacare Death Spiral". Bloomberg. January 18, 2017.
^ "Number of Insurers Participating in the Individual Health Insurance Marketplaces". Kaiser Family Foundation. January 30, 2017.
^ "CBO The Budget and Economic Outlook 2017–2027". CBO. 24 January 2017.
^ "Obamacare and Labor Supply". New York Times. June 20, 2015.
^ ab "Labor leaders' letter to Harry Reid and Nancy Pelosi". The Washington Post. January 27, 2014. Retrieved February 13, 2014.
^ ab "Union Letter: Obamacare Will 'Destroy The Very Health and Wellbeing' of Workers". The Wall Street Journal. July 12, 2013. Retrieved October 7, 2013.
^ Stolberg, Sheryl Gay (October 18, 2013). "States Are Focus of Effort to Foil Health Care Law". The New York Times. Retrieved October 19, 2013.
^ The Editorial Board (January 25, 2014). "The Koch Party". The New York Times. Retrieved January 25, 2014.
^ Peters, Jeremy (January 20, 2011). "Conservatives' Aggressive Ad Campaign Seeks to Cast Doubt on Health Law". The New York Times.
^ Chait, Jonathan (July 23, 2013). "Conservatives Brace for the Possibility Obamacare Won't Totally Suck". The New Republic.
^ Michael Cannon (July 6, 2007). "The Anti-Universal Coverage Club Manifesto". Cato Institute.
^ Chait, Jonathan (June 25, 2012). "Health Care As a Privilege: What the GOP Won't Admit". New York.
^ Schoen, John W. (November 9, 2016). "Here's what's coming from the Trump administration". CNBC. Retrieved November 16, 2016.
^ Haberman, Maggie; Pear, Robert (10 January 2017). "Trump Tells Congress to Repeal and Replace Health Care Law 'Very Quickly'". The New York Times. Retrieved 25 January 2017.
^ "Resolution 54: AFL-CIO Convention Resolution on the Affordable Care Act". AFL-CIO. September 11, 2013. Retrieved October 7, 2013.
^ Pradhan, Rachana (October 12, 2016). "Democratic governor: Obamacare 'no longer affordable' for many". Politico.
^ Demko, Paul (October 21, 2016). "Democratic governor expresses regret over Obamacare comments, requests emergency relief for rate hikes". Politico.
^ Cauchi, Richard (November 15, 2013). "State Legislation and Actions Challenging Certain Health Reforms". National Conference of State Legislatures. Retrieved November 28, 2013.
^ "Health Care Lawsuit Case Challenges". Independent Women's Forum. November 26, 2013. Retrieved November 28, 2013.
^ "March 14, 2012 Statement on Religious Freedom and HHS Mandate". United States Conference of Catholic Bishops. March 14, 2012. Retrieved April 28, 2012.
^ Goodstein, Laurie (May 21, 2012). "Catholics File Suits on Contraceptive Coverage". The New York Times.
^ Taylor, Audrey; Seanz, Arlette; Levine, Mike (June 25, 2015). "Supreme Court Upholds Obamacare Subsidies, President Says ACA 'Is Here to Stay'". ABC News. Retrieved June 25, 2015.
^ Haberkorn, Jennifer (May 12, 2016). "House GOP wins Obamacare lawsuit". Politico. Retrieved August 21, 2016.
^ Sargent, Greg (May 26, 2017), "Trump's latest tantrum will hurt hundreds of thousands of people. Here's how.", The Washington Post, retrieved 2017-05-29
^ Somashekhar, Sandhya (August 29, 2013). "States find new ways to resist health law". The Washington Post.
^ ab Ornstein, Norm (July 24, 2013). "The Unprecedented and Contemptible Attempts to Sabotage Obamacare". National Journal.
^ Pear, Robert (August 2, 2013). "Missouri Citizens Face Obstacles to Coverage". The New York Times. Retrieved August 3, 2013.
^ Cohn, Jonathan (July 25, 2013). "The Right's Latest Scheme to Sabotage Obamacare". The New Republic.
^ Kliff, Sarah (August 1, 2013). "Inside the Obamacare Resistance". The Washington Post.
^ O'Brien, Michael (March 22, 2010). "GOP quick to release 'repeal' bills". The Hill. Retrieved April 1, 2012.
^ "Bill Summary & Status – 112th Congress (2011–2012) – H.R. 2". THOMAS. January 19, 2011.
^ "Final Vote Results for passage of Repealing the Job-Killing Health Care Law Act (H.R. 2)". THOMAS. January 19, 2011.
^ Beutler, Brian (January 19, 2011). "Dems Press GOPers To Repeal Their Own Benefits Along With Health Care Law". Talking Points Memo. Retrieved January 21, 2011.
^ "Motion to Waive All Applicable Budgetary Discipline Re: McConnell Amdt. No. 13". U.S. Senate. February 2, 2011. Retrieved April 1, 2012.
^ "House Passes Health Care Repeal 245–189". C-SPAN. January 19, 2011.
^ Boles, Corey (June 28, 2012). "Romney, GOP Pledge to Repeal Health Law". The Wall Street Journal. Retrieved June 29, 2012.
^ "House Obamacare Repeal: Thirty-Third Time's the Charm?". ABC News. July 11, 2012.
^ Walker, Andrea K. (July 11, 2012). "House of representatives votes to repeal health reform for the 31st time". The Baltimore Sun. Retrieved July 12, 2012.
^ Deirdre Walsh (February 3, 2015). "House votes -again-to repeal Obamacare". Reuters. Retrieved February 4, 2015.
^ Jonathan Weisman; Robert Pear (May 26, 2013). "Partisan Gridlock Thwarts Effort to Alter Health Law". The New York Times. Retrieved May 27, 2013.we cannot use any of the normal tools to resolve ambiguities or fix problems
^ Lipton, Eric (March 19, 2013). "In Shift, Lobbyists Look for Bipartisan Support to Repeal a Tax". The New York Times.
^ Chait, Jonathan (July 3, 2013). "Obamacare Still Not Collapsing". New York.
^ Cohn, Jonathan (December 23, 2010). "What Defunding Health Reform Would Do". The New Republic.
^ Lori Montgomery; Paul Kane (October 1, 2013). "Shutdown begins: Stalemate forces first U.S. government closure in 17 years". The Washington Post.
Blake, Aaron (September 19, 2013). "McCain: Efforts to repeal and defund Obamacare 'not rational'". The Washington Post. Retrieved September 24, 2013.
^ Beutler, Brian (September 19, 2013). "New test could expose GOP's pack of charlatans". Salon. Retrieved September 24, 2013.
^ Cohn, Jonathan (August 7, 2013). "Tea Party to Republicans: Shut Down the Government, or You're a Sellout". The New Republic.
^ Goddard, Teagan (May 17, 2013). "Blocking the Medicare Reform Board Won't Stop Reform". WonkWire.RollCall.com. Archived from the original on September 21, 2013.
^ Cohn, Jonathan (May 24, 2010). "Save Donald". The New Republic.
Cohn, Jonathan (July 6, 2010). "Meet The Don". The New Republic.
^ Cohn, Jonathan (July 19, 2011). "The New Nullification: GOP v. Obama Nominees". The New Republic.
^ Kaplan, Thomas; Pear, Robert (12 January 2017). "Senate Takes Major Step Toward Repealing Health Care Law". The New York Times. Retrieved 12 January 2017.
^ "GOP Senate to Move Forward on ObamaCare Repeal". Fox News Politics. 11 January 2017. Retrieved 12 January 2017.
^ Lee, MJ; Barrett, Ted; LoBianco, Tom (12 January 2017). "Senate Opens Obamacare Repeal Drive with Overnight Marathon". CNN. Retrieved 12 January 2017.
^ Caldwell, Leigh Ann (12 January 2017). "Senate Approves First Step Toward Repealing Obamacare in Late-Night Session". NBC News. Retrieved 12 January 2017.
^ Golstein, Amy; DeBonis, Mike; Snell, Kelsey. "House Republicans release long-awaited plan to repeal and replace Obamacare". Washington Post. Retrieved March 7, 2017.
^ Pear, Robert (24 March 2017). "Push to Repeal Health Law Fails". New York Times. Retrieved 24 March 2017.
^ "House Republicans pass bill to repeal and replace Obamacare". CNN. May 4, 2017. Retrieved May 4, 2017.
^ "Senate Republicans signal they plan to scrap bill the House just passed and write their own".
^ Kaplan, Thomas; Pear, Robert (June 15, 2017). "Secrecy Surrounding Senate Health Bill Raises Alarms in Both Parties". New York Times. Archived from the original on June 18, 2017.
^ Bump, Philip (June 13, 2017). "The remarkable steps Republicans are taking to obscure what's in their health-care bill". Washington Post. Archived from the original on June 20, 2017.
^ Sarlin, Benjy; Caldwell, Leigh Ann (June 15, 2017). "The Senate's Health Care Bill Remains Shrouded in Secrecy". NBC News. Archived from the original on June 19, 2017.
^ "H.R. 1628, Better Care Reconciliation Act of 2017, discussion draft ERN17282" (PDF). Senate Budget Committee. June 22, 2017.
^ CNN, Lauren Fox, MJ Lee, Phil Mattingly and Ted Barrett. "McCain returns as Senate advances health bill". CNN. Archived from the original on July 25, 2017.
^ Klein, Ezra (July 28, 2017), The GOP's massive health care failures, explained, Vox, retrieved 2017-08-03
^ NYT-Steven Rattner-2017: The Year in Charts-December 29, 2017
^ ab "American Healthcare Act Cost Estimate" (PDF). Congressional Budget Office. March 13, 2017.
^ NYT-Edsall-Killing Obamacare Softly-July 27, 2017
^ The Coverage Gap: Uninsured Poor Adults in States that Do Not Expand Medicaid-October 19, 2016
^ ab Vox-Sarah Kliff-CBO: Trump is making Obamacare premiums more expensive-September 14, 2017
^ NYT-Robert Pear-Marco Rubio Quietly Undermines Affordable Care Act-December 9, 2015
^ Politico-Trump Still Enforcing Obamacare Mandate-May 2017
^ VOX-Sarah Kliff-Trump is slashing Obamacare's advertising budget by 90%-August 31, 2017
^ NYT-Editorial-Obamacare vs. the Saboteurs-November 4, 2017
^ Healthinsurance.org Ten Ways the GOP sabotaged Obamacare-May 17, 2017
^ Kodjak, Alison (October 13, 2017). "Halt In Subsidies For Health Insurers Expected To Drive Up Costs For Middle Class". NPR. Retrieved October 18, 2017.
^ Mulvihill, Geoff; Kennedy, Kelli (October 13, 2017). "Many states, consumers alarmed by Trump's health care order". Winston-Salem Journal. Associated Press. Retrieved October 18, 2017.
[permanent dead link]
^ ab Scott, Dylan (October 18, 2017). "Obamacare premiums were stabilizing. Then Trump happened". Vox.
^ "Sabotage Watch: Tracking Efforts to Undermine the ACA". Center on Budget and Policy Priorities. Updated October 12, 2017. Retrieved October 19, 2017.
^ Pear, Robert; Haberman, Maggie; Abelsonoct, Reed (October 12, 2017). "Trump to Scrap Critical Health Care Subsidies, Hitting Obamacare Again". The New York Times.
^ abcd Kliff, Sarah (October 18, 2017). "Sarah Kliff-Trump's stance on insurance 'bailouts' is completely incoherent" Vox..
^ ab "Federal Subsidies for Health Insurance Coverage for People Under Age 65: 2017 to 2027". Center on Budget and Policy Priorities. September 14, 2017.
^ ab "The Effects of Terminating Payments for Cost-Sharing Reductions". Center on Budget and Policy Priorities. August 15, 2017.
^ "A Town Hall, and a Health Care Model, in Green Bay". The White House Blog. Retrieved November 9, 2013.
^ Jacobson, Louis. "Barack Obama says that what he'd said was you could keep your plan 'if it hasn't changed since the law passed'". PolitiFact. Retrieved November 9, 2013.
^ "After the big Obamacare apology: where things stand". CNN. November 8, 2013. Retrieved November 9, 2013.
^ "Obama apologizes for insurance cancellations due to Obamacare". CNN. Retrieved July 29, 2014.
^ Obama blames 'bad apple' insurers for canceled coverage, Reuters.com, October 30, 2013.
^ Sealover, Ed (November 8, 2013). "Health insurers say they're canceling plans because of federal law". Denver Business Journal. Retrieved November 9, 2013.
^ "Lie of the Year: "If you like your health care plan, you can keep it". Politifact. December 12, 2014. Retrieved April 5, 2018.
^ Weigel, David (November 8, 2013). "The White House's Website Still Says If You Like Your Plan You Can Keep It". Slate. Retrieved November 9, 2013.
^ "Obamacare: The debacle". The Economist. November 2, 2013. Retrieved November 8, 2013.
^ "Obama apologizes to Americans who lost health plans". Fox News. November 8, 2013. Retrieved November 9, 2013.
^ Schoof, Renee (November 8, 2013). "Congress weighing laws to let people keep health insurance". McClatchyDC. Retrieved November 14, 2013.
^ ab "History of the Affordable Care Act (ACA)". October 22, 2014.
^ Enzi, Michael B. (August 2, 2011). "Health Care Reforrm Law's Impact on Child-Only Health Insurance Policies" (PDF). United States Senate. Retrieved August 10, 2016.
^ Liptak, Adam (September 30, 2012). "Supreme Court justices face important rulings in upcoming term September". The New York Times. Pittsburgh Post-Gazette. Retrieved September 30, 2012.
^ "Status of State Action on the Medicaid Expansion Decision". Kaiser Family Foundation. Retrieved August 12, 2016.
^ Walton, Alice G. "How To Explain The Obamacare Ruling To A Five-Year-Old". Forbes. Retrieved 5 May 2017.
^ "A Cruel Blow to American Families". The New York Times. February 2, 2013.
^ Cohn, Jonathan (February 5, 2013). "Not-So-Universal Health Care". The New Republic.
^ Mazur, Mark. "Continuing to Implement the ACA in a Careful, Thoughtful Manner". United States Department of the Treasury. Retrieved July 16, 2013.
^ Madara, Matthew R. (February 11, 2014). "ACA Employer Shared Responsibility Delay Included in Final Regs". Tax Notes Today. 2014 TNT 28–1.
^ Kennedy, Kelly (December 1, 2013). "White House claims success on HealthCare.gov repairs". USA Today. Retrieved December 1, 2013.
^ Cohen, Tom (October 23, 2013). "Rough Obamacare rollout: 4 reasons why". CNN. Retrieved November 5, 2013.
^ Holland, Steve; Rampton, Roberta (November 6, 2013). "Senate Democrats frustrated with botched rollout of Obamacare". The Christian Science Monitor. Reuters. Retrieved November 19, 2013.
^ Alonso-Zaldivar, Ricardo (July 31, 2014). "Probe exposes flaws behind HealthCare.gov rollout". AP News. Retrieved July 31, 2014.
^ Burwell v. Hobby Lobby, 573 U.S. (United States Supreme Court 2014).
^ Tracer, Zachary. "Obamacare Sign-Ups Decline to 10.2 Million as Some Don't Pay". Bloomberg.com. Retrieved August 21, 2016.
^ "December 31, 2015 Effectuated Enrollment Snapshot". cms.gov. March 11, 2016.
^ COOK, NANCY (December 16, 2015). "How the White House lost on the Cadillac Tax". Politico. Retrieved August 21, 2016.
^ "Supplemental Survey Report: Empire State Manufacturing Survey/Business Leaders Survey Firms Assess Effects of Affordable Care Act" (PDF). Federal Reserve Bank of New York. August 2016.
^ Mathews, Anna Wilde (August 16, 2016). "Aetna to Drop Some Affordable Care Act Markets". Wall Street Journal. ISSN 0099-9660. Retrieved August 16, 2016.
^ Ip, Greg (August 17, 2016). "The Unstable Economics in Obama's Health Law". Wall Street Journal. ISSN 0099-9660. Retrieved August 23, 2016.
^ "Louisiana to Expand Medicaid: Outlook for the States in 2016". Families USA. Retrieved August 22, 2016.
^ ab "Affordable Care Act signups dip amid uncertainty and Trump attacks". NYT. February 3, 2017.
^ Morton, Victor (February 14, 2017). "IRS weakens enforcement of Obamacare individual mandate: Report". The Washington Times. Retrieved 2017-02-16.
^ "House Passes Bill to Repeal Obamacare: Live Updates". WSJ. Retrieved 5 May 2017.
^ Epstein, Reid J. (5 May 2017). "Analyst Sees Danger for House Republicans After Health Bill Vote". WSJ. Retrieved 5 May 2017.
^ O'Brien, Elizabeth (December 2, 2017). "The Senate's Tax Bill Eliminates the Individual Mandate for Health Insurance. Here's What You Need to Know". Money.
^ Thomas Kaplan and Robert Pear. "2 Senators Strike Deal on Health Subsidies That Trump Cut Off".CS1 maint: Uses authors parameter (link)
^ "CBO says Trump's Obamacare sabotage would cost $194 billion, drive up premiums 20%". Vox. Retrieved 2017-10-17.
Further reading
Barr, Donald A. (2011). Introduction to U.S. Health Policy: The Organization, Financing, and Delivery of Health Care in America. JHU Press. ISBN 9781421402185.
CCH (2010). Law, Explanation and Analysis of the Patient Protection and Affordable Care Act: Including Reconciliation Act Impact. CCH Incorporated. ISBN 9780808022879. 1183pp
Feldman, Arthur M. (2011). Understanding Health Care Reform: Bridging the Gap Between Myth and Reality. CRC Press. ISBN 9781439879481.
Jacobs, Lawrence R.; Skocpol, Theda (2010). Health Care Reform and American Politics. Oxford U.P. ISBN 9780199781423.
McDonough, John E. (August 2, 2011). Inside National Health Reform. University of California Press. ISBN 9780520270190.
Brill, Steven (January 5, 2015). America's Bitter Pill: Money, Politics, Back-Room Deals, and the Fight to Fix Our Broken Healthcare System. Random House. ISBN 978-0812996951.
Heavey, Susan (February 18, 2011). "Repealing healthcare law would cost $210 bln: CBO". Reuters. Retrieved August 14, 2016.
"Letter to the Honorable John Boehner providing an estimate for H.R. 6079, the Repeal of Obamacare Act". Congressional Budget Office. July 24, 2012. Retrieved July 27, 2012.
"An Analysis of Health Insurance Premiums Under the Patient Protection and Affordable Health Care Act". Cbo.gov. November 30, 2009. Retrieved June 29, 2012.
"Analysis Of A Permanent Prohibition On Implementing The Major Health Care Legislation Enacted In March 2010". Congressional Budget Office. May 26, 2011. Retrieved April 1, 2012.
Glied, Sherry (December 2013). "How States Stand to Gain or Lose Federal Funds by Opting In or Out of the Medicaid Expansion" (PDF). Commonwealth Fund. Retrieved February 20, 2016.
"Paternalism 2.0". The Economist. August 23, 2014. Retrieved January 19, 2015.
Trish Riley; Jane Hyatt Thorpe. "Multi-State Plans Under the Affordable Care Act" (PDF). George Washington University Medical Center, Department of Health Policy. Archived from the original (PDF) on June 26, 2013.
"Beyond the pledges: Where the states stand on Medicaid". The Advisory Board Company. July 26, 2013. Retrieved August 27, 2013.
Sarah Kliff (May 5, 2013). "Florida rejects Medicaid expansion, leaves 1 million uninsured". The Washington Post (WP5513). Retrieved May 24, 2013.
Preliminary CBO documents
Patient Protection And Affordable Care Act, Incorporating The Manager's Amendment, December 19, 2009- Effects Of The Patient Protection And Affordable Care Act On The Federal Budget And The Balance In The Hospital Insurance Trust Fund (December 23, 2009)
- Estimated Effect Of The Patient Protection And Affordable Care Act (Incorporating The Manager's Amendment) On The Hospital Insurance Trust Fund (December 23, 2009)
Base Analysis – H.R. 3590, Patient Protection and Affordable Care Act, November 18, 2009.
(The additional and/or related CBO reporting that follows can be accessed from the above link)- Estimated Distribution Of Individual Mandate Penalties (November 20, 2009)
- Estimated Effects On Medicare Advantage Enrollment And Benefits Not Covered By Medicare (November 21, 2009)
- Estimated Effects On The Status Of The Hospital Insurance Trust Fund (November 21, 2009)
- Estimated Average Premiums Under Current Law (December 5, 2009)
- Additional Information About Employment-Based Coverage (December 7, 2009)
- Budgetary Treatment Of Proposals To Regulate Medical Loss Ratios (December 13, 2009)
CMS Estimates of the impact of P.L. 111-148
Estimated Financial Effects of the "Patient Protection and Affordable Care Act", as Amended. April 22, 2010.
Estimated Effects of the "Patient Protection and Affordable Care Act", as Amended, on the Year of Exhaustion for the Part A Trust Fund, Part B Premiums, and Part A and Part B Coinsurance Amounts. April 22, 2010.
CMS Estimates of the impact of H.R. 3590
Estimated Financial Effects of the "Patient Protection and Affordable Care Act of 2009", as Proposed by the Senate Majority Leader on November 18, 2009. December 10, 2009.
Estimated Effects of the "Patient Protection and Affordable Care Act" on the Year of Exhaustion for the Part A Trust Fund, Part B Premiums, and Part A and Part B Coinsurance Amounts. December 10, 2009.
Senate Finance Committee meetings
Senate Finance Committee Hearings for the 111th Congress recorded by C-SPAN[permanent dead link]; also available from Finance.Senate.Gov (accessed April 1, 2012).
External links
PPACA text
- Codification in U.S. Code is generally at 42 U.S.C. 18001 et sqq. To read it, start at GPO FDsys by selecting, in the Year menu, the most recent year that lists Title 42. In Title 42, seek section 18001 and subsequent sections.
- Public Law 111–148 after consolidating the amendments made by PPACA Title X and by HCERA.
Full text, summary, background, provisions and more, via Democratic Policy Committee (Senate.gov)
Public Law 111–148 U.S. Government Printing Office
